Briefing for Senedd debate on NHS waiting lists
Key points
Demand is increasing: The whole of the public sector is operating under severe pressure, with demand for services at an all-time high. While the long-term aim is to shift towards preventative and community-based services, the demand on frontline services remains extremely high.
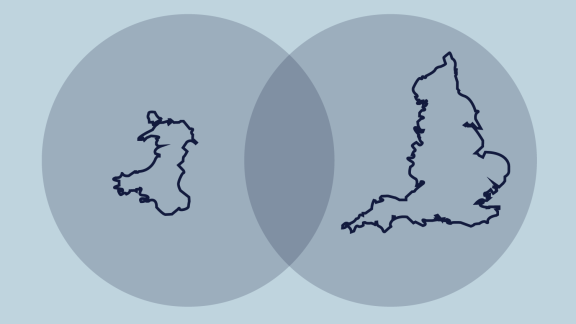
Performance measures across England and Wales: Data is collected, counted, coded and reported differently between the two nations. This means performance is not directly comparable and to give as accurate a picture as possible, every effort should be made to examine the context, including demographics and the health of the population, when making comparisons. For example, the population of Wales is proportionately older, poorer and sicker than that of England.
Social care: Challenges in social care have serious ramifications for patient flow through the health system and on the ability of the NHS to tackle the waiting list backlog. Social care services play a crucial role in care pathways, keeping people well for longer outside of hospital and enabling faster, safer discharges home. The sector plays a critical part in protecting NHS capacity and its ability to deliver high-quality, safe care. In May 2024, there were 1,624 adults occupying an NHS hospital bed who were ‘clinically optimised’, i.e. ready to return home or move on to the next stage of care. On average, the number of clinically optimised patients occupying beds equates to around 15% of all NHS hospital beds available.
Health and care workforce: We must acknowledge the relentless hard work of health and care staff and the care they do provide to thousands of people, day in, day out. Levels of activity are at record highs across most of the NHS. However, workforce is the number one limiting factor for NHS capacity. Recruiting and retaining staff is a priority, with wellbeing support, options for flexible working and upskilling all being considered by NHS leaders to effectively support existing staff while attracting new employees.
NHS estates and infrastructure: Across the UK it is vital that there is an increase in NHS capital spending to increase productivity and reduce waiting lists.
Engaging with the public: It is vital the Welsh Government, political parties and MSs are open with the public, so they understand the pressures facing the NHS and the need to radically re-think how services are delivered in the long-term. We continue to call for a national conversation and the creation of an open dialogue with the public about the future health and care services.
Demand is increasing
Demand for healthcare has grown significantly across the UK and will accelerate as the population continues to get older, with more complex health conditions and higher expectations of a longer healthy life. There’s no doubt the latest NHS activity and performance statistics for April and May make for sobering reading. NHS leaders are all too aware that this is not just a series of numbers on a page, but thousands of people’s lives being affected.
The statistics show sustained high levels of demand on the service, with NHS leaders telling us patients are more ill, and therefore needing more treatment, than ever before.
In May 2024:
• There was an average of 3,215 daily attendances to emergency departments, an increase compared to the previous month, and it was the highest number of emergency attendances on record.
• Just over 36,600 emergency calls were made to the ambulance service. This was an average of 1,182 calls per day, on average 87 more calls per day than the previous month, and 30 (2.6%) more per day than the same month last year.
• An average of 165 immediately life-threatening calls were made each day, 12 more than in April and the third highest on record. The number of immediately life-threatening 999 calls in May was 25% higher than the previous year and demand is nearly two-and-a-half times higher than pre-pandemic levels.
Performance measures across England and Wales
Waiting lists are a major challenge in both England and Wales and as our article “Can we make direct comparisons between the NHS in England and Wales?” demonstrates, the data we have needs to be put into context when making comparisons between England and Wales.
As highlighted in independent research, one reason for proportionately more people being on waiting lists in Wales is that its population is older, less healthy and with more people living in poverty – demographics that need proportionately more care and treatment.
We must remember that elective activity is just one area of health and care service delivery, making up one part of a much bigger system. Primary care, community care, social care, urgent and emergency care are just some areas where both countries will have varying performance measures which do not always easily compare.
Social care
Social care services play a crucial role in care pathways by keeping people well for longer outside of hospital and enabling faster, safer discharges home. ‘Pathway of care delays’ of adults occupying an NHS hospital bed, who are 'clinically optimised' ready to return home or 3 move on to the next stage of care, has a significant impact on patients, staff and on the flow of patients through hospitals, affecting the care available for others. It leads to patients being cared for in settings which are not the most appropriate to their needs and could introduce additional risks of harm to them, including hospital-acquired infections. It also has a knock-on effect on other NHS services. We also know the longer patients stay in hospital when they don't need to, the more likely they are to decondition and develop more advanced needs for care - particularly older, more frail patients.
As recent data highlights, in May 2024 there were 1,624 adults occupying an NHS hospital bed, who were 'clinically optimised', i.e. ready to return home or move on to the next stage of care. In April 2024, the number was higher at 1,738 - the highest it has been since April 2023. The number of patients occupying NHS beds who are clinically optimised and therefore ready to return home or move onto the next stage of care, as a proportion of estimated NHS hospital beds in Wales, is around 15%.
Being unable to discharge patients from hospital has a huge knock-on effect on NHS capacity. This is most visible in both ambulance response times and ambulance handover delays. This in turn can affect hospitals’ capacity to carry out scheduled care, such as hip and knee operations, restricting the NHS’s ability to tackle waiting lists.
NHS estates and infrastructure
The lack of capital funding and investment continues to impact NHS services in Wales and the rest of the UK. Some of the NHS estate was built before the NHS was founded – so over 75 years ago – which means a lot of NHS buildings are no longer fit for purpose and require millions of pounds in recurring maintenance costs. The current state of the estate has major implications on the physical capacity of the NHS to make inroads into planned care backlogs, limiting levels of activity and its ability to become more efficient.
Capital investment is key to continuing to deliver high-quality, safe health services, as well as reaching longer-term goals to deliver innovation and integrate care. Without reshaping NHS estates and infrastructure, the sustainability of NHS estates is compromised. This means it’s difficult to boost productivity, supporting the NHS to get through its care backlog, reduce carbon emissions, maximise public assets, attract additional funding through research and development opportunities, regenerate the local economy and improve patient outcomes.
The need for a national conversation
As highlighted in our briefing, The NHS at 75: How do we meet the needs of future generations?, politicians must communicate the scale of the challenge for the health and care system to the public. We need an open and honest conversation about what the NHS can be expected to provide in the future. Difficult decisions will have to be made between the demands of elective recovery, access to primary care, mental health and the generational task of reducing health inequalities. That is why NHS leaders require the Welsh Government, and all politicians, to be clear with the public about the scale of the recovery challenge. There is a need to engage with the public on choices required, as the model for long-term service delivery will take time to implement, so short-term measures will need to be established to deliver higher priority services.
The public must feel personally invested in their wellbeing and our health and care service to help ensure its long-term sustainability, which will only be possible through public involvement and co-production of services. This will allow people to feel supported, empowered and informed about their health and wellbeing, manage their conditions and use services responsibly.
Conclusion
Creating a sustainable health and care system requires a cross-sector effort to build healthier and more prosperous communities, reducing demand well into the future. We cannot lose sight of the fact that this is not about budgets, targets and deficits – it is about people’s lives.
We need commitments from governments and political parties to longer term thinking, including focusing on prevention, shifting more care into the community, capital investment to make NHS estates more efficient and ringfenced investment so social care staff can have parity of pay. Without this, we cannot expect to see the meaningful change we all want to see.
Further information
If you would like further information on any of the issues raised in the briefing, please contact Nesta Lloyd-Jones on nesta.lloyd-jones@welshconfed.org
The Welsh NHS Confederation represents the seven Local Health Boards, three NHS Trusts (Velindre University NHS Trust, Welsh Ambulance Services University NHS Trust and Public Health Wales NHS Trust), and two Special Health Authorities (Digital Health and Care Wales and Health Education and Improvement Wales). The twelve organisations make up our members. We also host NHS Wales Employers.