Key points
While the genesis of this report is multifaceted, the overarching purpose is to evidence the costs of various women’s health conditions, when left sidelined, to the overall economy; showcase the potential return on investment (ROI) for every additional £1 that is invested in women’s health services throughout the NHS; and to assess the state of women’s health inequalities throughout the country to inform where additional public investment should be directed.
Our findings illustrate that:
for every additional £1 of public investment in obstetrics and gynaecology services per woman in England, there is an estimated ROI of £11. If an additional £1 per woman in England were invested in these services, the economy could benefit from an additional £319 million in total gross value added (GVA)
the economic cost of absenteeism due to severe period pain and heavy periods alongside endometriosis, fibroids and ovarian cysts is estimated to be nearly £11 billion per annum
unemployment due to menopause symptoms has a direct economic impact of approximately £1.5 billion per annum with approximately 60,000 women in the UK not being in employment due to menopause symptoms
local authorities throughout England with higher ethnic diversity were found to have poorer access to women’s health services
local authorities throughout England with higher levels of deprivation were found to report worse women’s health outcomes
systems classified as ‘high investors’ in obstetrics and gynaecology services saw fewer NHS staff sickness absences compared to the ‘low investors’, highlighting the positive impact of women’s health investment on the NHS workforce
there are several correlations between gynaecological conditions, poor physical health (ie multimorbidity), and mental ill health (ie multimorbidity), with nearly half of women reporting that while they did not take time off work as a result of a gynaecological health condition, they would have liked to
of those with long-term physical or mental health conditions, 83 per cent of women reported the condition having a negative impact on their ability to go to school, college or university; perform work for a family business; look for work; or look after the family and home.
In the recommendations section of this report, we outline our asks to key national bodies – including HMT, DHSC, NHSE, NIHR, and the ONS – who hold many of the key levers pivotal to closing the gender health gap at pace. Our recommendations include:
allocating ringfenced funding to support the remaining eight years of the Women’s Health Strategy for England
distributing additional funding according to variations in need throughout the country and appointing an ambassador for women’s health focused specifically on improving outcomes for black, Asian, and minority ethnic women
committing to annual increases in the allocation of public research funding to conditions that affect men and women alike albeit differently or disproportionately in addition to conditions that only affect women
collecting disaggregated data that captures the intersecting inequalities of women’s lives such as race, socioeconomic status, and ability and making it publicly available
refurbishing education and training for medical professionals specific to conditions that solely affect women as well as those that affect women differently.

Introduction
The UK health and social care system, like many others worldwide, was designed around a white, cis-gender, heterosexual, male prototype. However, the UK stands out as the country with the largest female health gap in the G20 and the 12th largest globally, with women spending three more years in ill health and disability when compared to men. The ‘male default’ permeates research, clinical trials, education and training, as well as the design of policies and services. Gender bias in medicine is therefore not only scientific or biomedical, but also social, cultural and political.
Numerous reports indicate the deeply entrenched and systemic nature of this gender health gap. Baroness Julia Cumberledge’s report First Do No Harm investigates the devastating impact of hormone pregnancy tests, sodium valproate, and pelvic mesh implants – treatments and devices all taken or used by women, which have been linked to birth defects, pregnancy losses, physical malformations and developmental delays in children. The report describes a ‘widespread and wholly unacceptable labelling of so many symptoms as ‘normal’ and attributable to ‘women’s problems’. This reported culture of ‘dismissiveness’, ‘arrogance’ and ‘defensiveness’ is underscored further in the Women’s Health – Let’s Talk About It survey, revealing that out of nearly 100,000 respondents in England, 84 per cent reported having been dismissed by medical professionals.
The Royal College of Obstetricians and Gynaecologists’ (RCOG) report Left For Too Long, cites that gynaecology was one of the worst affected specialisms during the COVID-19 pandemic, experiencing the highest percentage increase of any speciality. Indeed, gynaecology waiting lists increased substantially across all four nations of the UK between the start of the pandemic and winter 2021/22, with these increases ranging between 42 per cent in Northern Ireland, 60 per cent in England, 62 per cent in Wales, and 95 per cent in Scotland. The report highlights that ‘… a general lack of bed capacity across hospitals, combined with the low priority given to elective gynaecology, means that surgical activity in gynaecology is often one of the first to be scaled down when bed occupancy is high’.
These issues show no signs of abating: a gynaecology care crisis was underscored again in July 2024, with nearly half (46 per cent) of those on waiting lists falling beyond the NHS target of 18 weeks and nearly 30,000 women waiting for over a year. The consequences of this deprioritisation of women’s health services continue to be felt heavily throughout the system, with extensive waiting times levying far more advanced conditions for patients, including organ prolapse, sepsis, kidney failure, and cancers left undiagnosed, resulting in more complex, labour-intensive and thereby costly interventions.
Unfortunately, there is a plethora of data showcasing how the NHS often fails to serve 51 per cent of the population; these references point to only a fraction of the documentation showcasing the systemic, operational, structural and cultural shortcomings of the health system as it pertains to women’s health. Rather than continuing to delineate women’s health inequalities and the consequences that they present to society, this paper approaches them through an analytical economic lens to inform the wider health policy landscape.
We assess a range of conditions at a macro level, unpacking the interdependencies across women’s health and the consequences of not treating one condition efficiently and effectively, which can exacerbate the original condition and spawn other health problems. Our return-on-investment analysis will show that while addressing existing inequalities across women’s health services will require an initial investment, this expense is relatively modest compared to the growing costs incurred by both the NHS and wider society as direct consequence of continuing to neglect the health outcomes of the 51 per cent.
As part of this project, we invited those with lived experience of primary dysmenorrhea, fibroids, polycystic ovary syndrome (PCOS), endometriosis, adenomyosis, the menopause, and infertility to participate in discussions to speak about their health journey. With their permission, we have included a range of anonymised quotes throughout the report to highlight the people behind the statistics. It is their experiences that keep us pushing for the policy changes that we have suggested herein.
Language
‘Women’s health’ is often portrayed in a myopic way which represents a quintessential cisgender, heterosexual, able-bodied, white woman. However, sexism in medicine intersects countless forms of discrimination, including racism, ageism, transphobia, homophobia, classism, and ableism, and these systemic biases affect all of us. Where the data has allowed, we have pointed to variations in women’s health according to, for instance, ethnic diversity and socioeconomic status. Where we use the terms ‘woman’, ‘women’, ‘female(s)’, or ‘women’s health’ throughout this report, our intention is that these terms are understood to represent all women, while recognising the shortcomings of the health system’s data in representing the rich diversity within this group of people. We also acknowledge that some of these services and experiences are not limited to cis-women but also affect gender diverse communities and intend our findings to be read in this context.
As this study assesses the relationship between women’s health and the economy, the predominant element through which we measure economic impact is the labour market. Unless specified otherwise, when referring to employment, work, or labour, we are assessing formal work. This orthodox view of ‘work’ is largely a result of scarce data and lack of valuation around unpaid and informal work 1 alongside the reliance on standard measures of economic performance, such as GVA, which have historically neglected the value that unpaid and informal work1 add to the economy. In the realm of health economics, this exclusion is particularly problematic given the crucial role that informal and unpaid carers play in plugging the gaps of health and social care. Moreover, in a study specific to women’s health, recognising the disproportionate amount of unpaid and informal labour that women undertake when compared to men, 2 this is a critical topic that merits attention.
The term ‘conditions’ refers to diseases, and only when citing external sources to physiological processes (eg menopause), in order to maintain consistency with the data leveraged throughout the analysis. This terminology should not be interpreted to reinforce a medicalised perspective or allude to any inherent ‘wrongness’ with women’s health across the life course, as experiences vary greatly among women and medical interventions may not always be required. Moreover, the use of ‘reproductive health’ to encompass all gynaecological conditions can be reductionist, excluding or inherently deprioritising those who do not wish to or are unable to reproduce, and we have only used this term when referring to external sources. Overall, we aim to maintain consistency with the language used in our sources and endeavour to approach these topics with sensitivity and advocate for a more nuanced understanding of all aspects of women’s health.
Chapter footnotes
Policy context
In July 2022, the DHSC published England’s first women’s health strategy. The ten-year strategy sets out a myriad of ambitions for improving the health and wellbeing of women and girls throughout England based on a life course approach. The vision includes ensuring that the voices of women and girls are heard, improving access to services, addressing disparities in outcomes, promoting better information and education, cultivating an increased understanding of how women’s health impacts workplace experiences, and supporting more research and better data. These ambitions are robust and lay a foundation for significant improvements in the health of women and girls across the country.
On International Women’s Day (8 March 2023), the former minister for women’s health announced a £25 million investment to support the establishment or expansion of women’s health hubs 3 throughout the country. However, the letter addressed to integrated care board (ICB) chief executives outlining the fine print of the investment explicitly states:
‘The £25 million investment announced in March will be distributed equally to ICBs, with £595,000 in total for each ICB. This will be transferred over the current and next financial year (that is, 2023 to 2024 and 2024 to 2025), with 75 per cent available in 2023 to 2024 for immediate use. We encourage you to make full use of your funding allocation to accelerate progress, noting that ICBs will not be expected to incur costs implementing a model that is not recurrently affordable.’
Immediately apparent in this specification was the notion that a key tenet of the ambitious ten-year Women’s Health Strategy – the women’s health hubs – had only two years of funding to support delivery, and as a result could not amount to much more than a time-limited ‘proof of concept’ in already over-burdened and financially strapped systems. Despite the DHSC’s evidence highlighting that for every £1 spent on implementing a PCN-sized hub, there are estimated to be £5 of benefits, alongside the general enthusiasm for the strategy, several ICB leaders noted that the limited and short-term resources would be depleted before the ROI benefits could be realised. Compounding this gridlock, NHS England issued a letter to ICB leads in November 2023, only weeks after the distribution of the women’s health funding, requiring a plan indicating how systems will ‘deliver financial balance’ by the end of the financial year in light of significant industrial action. Assessing the nonrecurrent and limited nature of the allocated women’s health funding, many systems made the difficult decision to rescind their women’s health budgets altogether to plug preexisting deficits.
As the end of the current (2024/25) financial year approaches, questions remain about the support ICBs will receive to further the implementation of the Women’s Health Strategy and gender health equity more broadly. Now is therefore the time to showcase the full nature of this issue and its importance to the nation. The intention of this report is to make the case to the centre – mainly HMT, the DHSC, and NHS England – that women’s health, including the Women’s Health Strategy, is not only a just investment, but it’s also an economically savvy one. It is time for the centre to evidence that it not only understands the gravity of gender health gap across the UK, but that they are committed to closing it. It is time for government to invest in the 51 per cent.
Chapter footnotes
- 3. Womens Health Hubs are intended to be ‘one-stop-shop’ models of care in the community – working at the interface of primary and secondary care – that streamline a range of specialist services, including but not limited to contraception, screening, menstrual health, and the menopause, improving access and quality of care while boosting efficiencies. ↑
Approach
The decision to focus predominantly on the ROI of boosted resource in obstetrics and gynaecology services was deliberate, given the Women’s Health Strategy is mainly focused on sexual health and gynaecology, and this piece’s principal aim is to evidence the benefits of fully funding this ten-year plan. While these areas are important, women’s health spans far beyond this sphere. There are conditions that affect women differently than men such as cardiovascular disease, conditions that affect women disproportionately such as autoimmune diseases, osteoporosis, and migraines, and countless conditions where sex differences are not yet known.
The McKinsey Health Institute and World Economic Forum’s report Closing the Women’s Health Gap: A $1 Trillion Opportunity to Improve Lives and Economies estimates that women-specific conditions – mainly maternal and gynaecological – account for 5 per cent of the global women’s health burden, while 56 per cent of this burden is attributed to conditions that affect women differently or disproportionately. In the mapping of women’s health inequalities throughout the country, we have touched upon broader indicators such as mental health, autism, and learning disability services; healthy life expectancy and disability free life expectancy; avoidable mortality; and sickness absence. Still, this piece unpacks only a sliver of what constitutes women’s health.
“We make up 51 per cent of the population, yet our needs are largely ignored.”
Setting out the boundaries of this analysis hopefully elucidates the amount of work left to do – across geographies, conditions, and themes in addition to services, such as research
4
5
and innovation.
6
It is not our intention to answer every question that relates to investment in women’s health, but rather, to contribute to a very nascent conversation and shed light on opportunities to further this critical work.
Chapter footnotes
- 4. Approximately 2 per cent of overall public research funding is dedicated to reproductive health and childbirth, and this number has not shifted in the past decade (UK Health Research Analysis). ↑
- 5. For instance, Women’s Health Access Matters (WHAM) calculates that investing $350 million in women’s health research across Alzheimer’s disease and Alzheimer’s disease–related dementias, coronary artery disease, rheumatoid arthritis, and lung cancer portfolios generates a $14 billion ROI to the US economy. These results suggest that modest increases in funding for women’s health research have the potential to yield very large gains. ↑
- 6. The McKinsey Health Institute and World Economic Forum’s report cites that ‘Approximately 1 per cent of healthcare research and innovation is invested in female-specific conditions beyond oncology. In the digital healthcare space, FemTech companies received 3 per cent of the total digital health funding’. ↑
Analysis
This women’s health economics analysis is comprised of three key pillars: a longitudinal assessment of select gynaecological health conditions on labour market outcomes, the potential ROI of further investment in obstetrics and gynaecology services across England, and an assessment of women’s health inequalities throughout the country. The narrative that this sequence follows underscores the extent to which women’s health conditions – if left untreated or disregarded – can negatively affect the labour market and wider economy; the potential economic growth that the country could realise through boosted investment in women’s health services; and finally, an assessment of how additional investment in women’s health services could be more inclusive. In this format, we highlight the gravity of the gender health gap in economic terms, evidence the extent to which further investment could boost economic growth, and finally, discuss the nuances around investment and some of the factors beyond funding that are equally necessary to closing the gender health gap in England.
A longitudinal assessment of select conditions on labour market participation
With estimates indicating that women account for approximately 49 per cent of the formal (paid) workforce, and undertake a disproportionate amount of informal 7 (unpaid) labour in comparison to men, it is undeniable that women’s overarching contributions to the economy are substantial. However, women represent a disproportionate amount of those out of formal work and economically inactive, attributing the main cause of economic inactivity to long-term sickness (figure 1).
Moreover, while sickness absence rates have been on the rise for both women and men since 2020, they are 1 percentage point higher in women than in men (figure 2).
While these statistics are solely representative of formal work, it is important to understand the impact that long-term conditions can have on the informal sector. From the Reproductive Health Survey (RHS), we found that for those with a long-term physical or mental health condition:
- Of those going to school, college or university full-time, 82.5 per cent reported that the condition reduced their ability to carry out day to day activities.
- Of those doing unpaid work for a family business, 80.8 per cent reported that the condition reduced their ability to carry out day to day activities.
- Of those intending to look for work but were prevented from doing so by temporary sickness or injury, 95 per cent reported that the condition reduced their ability to carry out day to day activities.
- Of those looking after the home or family, 73.2 per cent reported that the condition reduced their ability to carry out day to day activities.
However, it is difficult to determine the specific health issues driving these trends due to the lack of granularity in rationale collected by the ONS. Given the occurrence rate of those who selected ‘other’ illness as a cause for sickness absence preceding and following the height of the COVID-19 pandemic, 8 as represented in figure 3, 9 alongside the evidence outlined in this report surrounding the prevalence of gynaecological health conditions and their impact on women’s participation in the labour market, we have included a recommendation to the ONS to collect better information as it relates to gynaecological health.
Methodology 10
Given the lack of data surrounding the impact that gynaecological and reproductive health conditions have on labour market participation, to conduct this portion of the econometric analysis, two key data sources were leveraged: the British Cohort Study (BCS) and the RHS. 11 The conditions we opted to assess econometrically include primary dysmenorrhea, 12 secondary dysmenorrhea, 13 as well as perimenopause and menopause. 14 15 These conditions were selected given their prevalence as well as data availability. We additionally conducted a descriptive analysis surrounding infertility and its impact on mental health outcomes. The entirety of this longitudinal analysis was performed at the individual level, which allowed us to control for observable personal characteristics such as education, occupation and overall health status. Moreover, given the longitudinal nature of this assessment we were able to compare outcomes both prior to and following the condition, which allows us to evidence causality.
Three outcome variables are considered to measure the results. First, labour market outcomes are assessed by using a dummy variable 16 indicating whether the individual is in employment or not. Second, mental health outcomes are proxied by using a variable showing whether the individual reported ‘regularly feeling miserable or depressed’ in the BCS. Third, physical health is indicated through a self-assessment of the respondents’ health, comparing those that state that their health is ‘poor or fair’ to those that report ‘good, very good or excellent’ health. The results outlined below are represented in terms of absenteeism, which is measured by days of missed work and presenteeism, 17 which is characterised by lower levels of productivity.
Findings
1. Primary and secondary dysmenorrhea
For those in employment, the RHS shows that those experiencing both primary and secondary dysmenorrhea are more likely to miss work due to period-related symptoms. On average women with:
- Women with severe period pain miss 18 days of work per year due to their symptoms.
- Women with heavy periods miss 11 days of work per year due to their symptoms.
- Women with secondary dysmenorrhea miss 16 days of work per year due to their symptoms.
- 30 per cent of those experiencing endometriosis take more than three days off per month due to period pain, compared to 6 per cent of those who do not experience endometriosis.
“In the 15 years that I have suffered with endometriosis, I would say that I’ve seen a doctor well over 100 times. During the worst five years leading up to my diagnosis, I was visiting the GP at least once if not twice a month.”
If we assume that the RHS is representative of people experiencing primary and/or secondary dysmenorrhea, we can estimate their economic impact of absenteeism. By using the ONS data (2023) on median annual gross pay for females aged 16-45, we estimate the following economic impact: 18
- The impact of absenteeism due to severe pain during periods: £3.7 billion per year.
- The impact of absenteeism due to heavy periods: £4.7 billion per year.
- The impact of absenteeism due to secondary dysmenorrhea: £2.2 billion per year.
“I faint at work regularly throughout the day and have to change my clothes up to four times when menstruating. I cannot take time off for it as there is no explicit workplace support for fibroids and periods. My time off has been due to catastrophic bleeds and hospitalisations, usually for a few weeks to a few months at a time.”
Findings from the RHS indicated that 40 per cent of women with severe period pain, 45 per cent of women with heavy periods, and 40 per cent of women with secondary dysmenorrhea reported that they wanted to take time off work as a result of their condition but did not.
As above, by using the most recent data on median annual gross pay for women aged 16-45, we estimate the economic loss due to presenteeism:
- The impact of presenteeism due to severe pain during periods: £291.9 million per year.
- The impact of presenteeism due to heavy periods: £418.1 million per year.
- The impact of presenteeism due to secondary dysmenorrhea: £173.0 million per year.
“I don’t take sick days but I often arrive late or am not fully present, so my work is not as good as a day when I’m not dealing with these issues.”
BCS data analysis indicates that those experiencing primary dysmenorrhea were found to be 7 percentage points 19 more likely to be ‘miserable or depressed’ than the rest of the population. This is equivalent to an additional 340,000 women experiencing poor mental health in the UK specifically related to primary dysmenorrhea. Moreover, a significant relationship between both primary and secondary dysmenorrhea and physical health can be seen from the econometric analysis: those with primary dysmenorrhea are 2 percentage points more likely to be in ‘poor’ or ‘fair’ health, and those with secondary dysmenorrhea are 6 percentage points more likely to be in ‘poor’ or fair’ health. Combined, this is equivalent to an additional 260,000 women experiencing ‘poor’ or ‘fair’ health. The RHS corroborates these results, finding that those experiencing dysmenorrhea are more likely to report worse levels of overall health. For example, those with secondary dysmenorrhea were five times as likely to report their health status as ‘bad’ or ‘very bad’ compared to the rest of the population (15 per cent compared to 3 per cent).
“There were times when I was using multiple products when I was in a meeting. Still, the entire time, I was fearful that something might happen. I think this highlights how lonely it can feel because it’s invisible to everyone else and it really does affect your confidence. It’s all you can think about when you are in a public place or a meeting worrying about the embarrassment of an incident.”
Poor mental health and physical health are both associated with significant negative economic impact. The Mental Health Economics Collaborative found that the total cost of mental ill health in England in 2022 was £300 billion, which is comprised mainly of losses to the economy – for example due to sickness absence or presenteeism – and human costs in terms of quality of life. However, due to the nature of the questions used in the BCS, we cannot quantify the resulting economic impact of the reported poor mental health.
“I simply could not have carried on living in the amount of pain I was in and the thought of another two years of it pushed my mental health to breaking point.”
2. Perimenopause and menopause
This analysis operates under the notion that those experiencing perimenopause and menopause symptoms are typically aged 46 – 55, which amounts to approximately 4.5 million women. 20 Data from the BCS is used to determine the proportion of these women that experienced ‘less severe’ 21 (one-to-two symptoms) 22 or ‘more severe’ (three-to-four symptoms) perimenopause and menopause. Capturing perimenopause and menopause severity beginning at age 46 might be a cautious estimate as many women at this age may not have begun the menopause transition, but due to a lack of better data, this is the age range that was selected.
Drawing upon data in the BCS, we identified a significant causal relationship between employment and more severe menopause (ie experiencing three-to-four symptoms): women with severe menopause are 5 percentage points less likely to be in employment compared to the rest of the population. Similar findings were identified in the RHS, which collected data on eight menopause symptoms. 23 When compared to those experiencing just one menopause symptom, those with all eight menopause symptoms were 6 percentage points less likely to be in employment (83 per cent compared to 89 per cent), and twice as likely to be economically inactive due to health reasons (8 per cent compared to 4 per cent). Those in employment and experiencing eight menopause symptoms were also much more likely to miss work due to menopause symptoms, with 20 per cent reporting that they generally took time off each month due to the menopause. This is compared to 3 per cent of those experiencing one menopause symptom. Although 20 per cent of those with eight symptoms did take time off, most of this group did not take time off due to the menopause. Of the majority that took no time off due to menopause symptoms, over three-quarters (76 per cent) of them reported that they had wanted to.
“The only reason I don’t take sick days is because I work from home. If I didn’t, I would have to take about six months a year off.”
Based on these findings from the BCS, there are an additional 60,000 women not in employment as a result of the perimenopause or menopause. If those women were to enter employment, earning the average wage of a woman of menopausal age in employment, 24 this could generate an increase in direct economic impact of approximately £1.5 billion per annum. This figure does not consider other economic factors such as savings in terms of reduced welfare payments, the indirect and induced impact associated with any increases in income (ie the ‘ripple effect’ caused by individuals spending more money), or the savings employers realise in not having to hire and train new employees.
“I felt isolated and lonely. In March 2016 I ended up leaving my employer of 23 years because my menopause was not supported.”
Findings from the RHS indicate that, on average, women with severe menopause symptoms take seven days off work per year due to their symptoms, and around 60 per cent of women want to take days off work for their menopause symptoms but do not. Employing the methodology that was used above to estimate the impact of dysmenorrhea on absenteeism and presenteeism, we estimate the economic impact of absenteeism due to severe perimenopause and menopause symptoms to be £191.0 million per year and the economic impact of presenteeism due to severe perimenopause and menopause symptoms to be £22.4 million per year.
In terms of mental health, the econometric analysis found significant impacts associated with both treatment groups. Those experiencing one-to-two perimenopause and menopause symptoms were 9 percentage points more likely to regularly feel ‘miserable or depressed’, which increased to 17 percentage points when considering those with three-to-four perimenopause and menopause symptoms. Overall, this is equivalent to an additional 370,000 women experiencing poor mental health due to the perimenopause and menopause.
In regard to physical health, the econometric analysis finds that those with more severe perimenopause and menopause are 15 percentage points more likely to report that their health is ‘poor’ or ‘fair’ compared to the rest of the population.. This is equivalent to an additional 210,000 women experiencing worse health outcomes due to the perimenopause and menopause. The findings from the RHS show that those experiencing all eight menopause symptoms are almost twice as likely to report that their health is ‘bad’ or ‘very bad’ compared to those experiencing one menopause symptom (11 per cent compared to 6 per cent). Given the limited nature of the survey questions in this category, the compounding mental and physical health impacts cannot be quantified in monetary terms, but the wider literature shows the substantial impact that poor mental health can have on the economy.
3. Infertility and perinatal loss
It is widely recognised that both infertility and perinatal loss can have a tremendous impact on mental health. Fertility Network UK commissioned a survey (2022) of fertility patients across the nation and found that almost half of respondents experienced feelings of depression either often or all the time. Researchers at the University of Edinburgh conducted a systematic review and meta-analysis of perinatal loss (2021), finding that women who experienced perinatal loss were twice as likely to experience depression and one and a half times more likely to experience anxiety in comparison to the rest of the population.
“I really want employers and health services to recognise that the grief can be overwhelming and significantly impact mental health.”
The economic impacts of infertility and perinatal loss could not be explored in the main econometric analysis due to low sample sizes in the survey data. However, making use of the longitudinal nature of the BCS, we assess the impact that infertility has on mental health outcomes throughout the life course. The analysis makes use of a question asked regarding fertility status, when respondents are 30 years old. It considers those who answered that they:
- 'have been sterilised or have had a hysterectomy'
- 'have been told that they are unable to have children' or
- 'have been advised not to have children'.
It then compares this sample to the population as a whole.
We found that 37 per cent of this sample population report that they often feel ‘miserable or depressed’. In comparison, 22 per cent of the population as a whole report poor mental health, representing a difference of 15 percentage points. The difference between these groups remains in later waves of the study. For example, at age 46 (wave 10), 40 per cent of those that were unable to have children at age 30 report poor mental health, compared to roughly a quarter (24 per cent) of the sample.
The case for investment in obstetrics and gynaecology services
As the previous section illustrates the impact that select conditions can have on individuals and the wider economy, this portion of the report focuses on the potential economic growth – measured through GVA – that could be realised by investing further in obstetrics and gynaecology services. It is important to note that given the siloed nature 25 of service commissioning – particularly with various sexual health services falling under the purview of local authorities – obstetrics and gynaecology services alone do not encapsulate the breadth of the topic, 26 however they do provide a sensible evidence base.
Methodology 27
To quantify the economic impact of further public investment in obstetrics and gynaecology services 28 throughout England, we examined the relationship between geographical and temporal 29 changes in investment alongside corresponding economic performance. The indicators for economic performance assessed included GVA per head, 30 which is utilised to define the ROI, female employment rate, and NHS sickness absence rates. 31 GVA and female employment rate were assessed to investigate the extent to which investing in obstetrics and gynaecology services could boost productivity and economic output under the assumption that more investment could promote earlier diagnoses and treatments, allowing more women to lead healthy and productive lives. NHS sickness absence was investigated under the same assumption, while additionally accounting for the role it plays as the UK’s largest employer alongside the ‘ripple effect’ that the NHS workforce has in regard to economic prosperity (ie the part it plays in keeping the wider population healthy, productive, and economically active).
To control for the confounding effect that Brexit and the COVID-19 pandemic could have on performance indicators, the analysis relied on data collection prior to this period (2014/15 to 2018/19). Due to a lack of data on expenditure in NHS obstetrics and gynaecology services, it was necessary to construct a proxy to measure expenditure in obstetrics and gynaecology services by clinical commissioning groups (CCGs) 32 which relied on the proportion of staff costs in these practice areas across community and secondary care settings 33 when compared to all practice areas within the geographic area covered by respective CCGs.
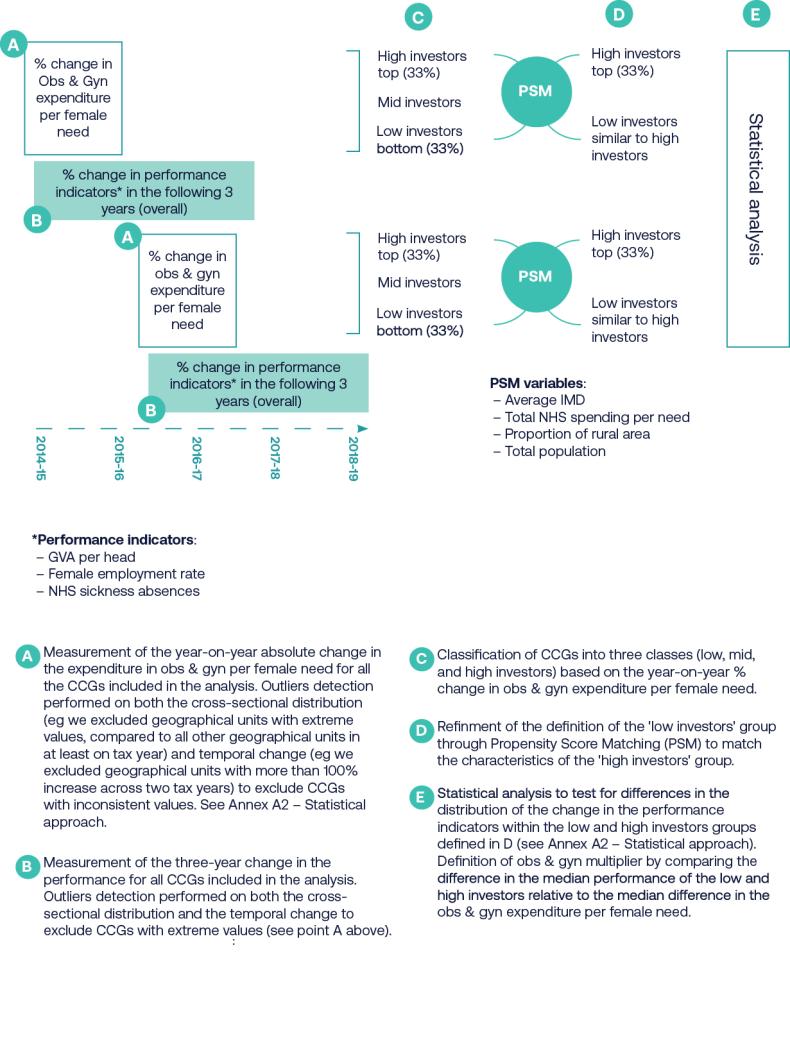
To investigate the link between public investment in obstetrics and gynaecology services and economic performance indicators, a statistical approach was employed, which compared the economic performance of CCGs with high investment in obstetrics and gynaecology services to those with low investment. 34 Due to a potential delay in the effects of this public investment, we examined changes in economic performance during the three following tax years. Propensity score matching (PSM) was applied to align CCGs in the high-investor group to CCGs in the low-investor group with similar characteristics including total NHS expenditure relative to need, total population, the proportion of the population living in a rural environment, and the average deprivation level of the area. 35 Finally, we compared the changes in economic performance indicators between CCGs classified as high and low investors. An outline of this approach is presented schematically in figure 4.
Figure 4: Approach to comparing economic performance indicators between CCGs classified as high and low investors
Findings
- While NHS sickness absences increased for both high- and low-investing, CCGs across the time period, we found a statistically significant difference between CCGs classified as high and low investors and NHS sickness absences. Specifically, considering median values, the increase in NHS sickness absences rates was 0.9 percentage points for low-investor CCGs compared to 0.3 percentage points for high-investor CCGs, indicating that CCGs that invested more in obstetrics and gynaecology services experienced fewer NHS staff sickness absences.
- We did not find a statistically significant difference in the three-year variation in female employment rate between high- and low-investing CCGs, which aligns with results outlined in the previous analysis specific to dysmenorrhea. The overall female employment rate will not account for sickness absences, changes in the number of inactive women who join the labour market after a period of economic inactivity, labour market participation arising from part-time to full-time work transitions or boosted productivity as a result of additional investment.
- In terms of GVA, we found that CCGs classified as 'high investors' experienced statistically significant additional growth in GVA per capita in the following three years compared to similar CCGs classified as ‘low investors’. We calculated that an increase of £319 million in the total GVA could have occurred had an additional £1 been invested in community and acute obstetrics and gynaecology services per female in England. This suggests a ROI of £10.90 for each additional pound spent per female in England.

An assessment of women’s health inequalities throughout England
Thus far, we have demonstrated the extent of the economic impact of certain women’s health conditions alongside the potential ROI of boosted resource. However, this paper would be remiss if it assumed that investment alone would close the gender health gap, or that further investment should be distributed equally throughout the country. As such, this final pillar of the analysis assesses the variation in access to women’s health services and health outcomes as well as their connection to socioeconomic conditions and ethnic diversity across local authorities in England.
Methodology 36
To provide an overall measure of access to women’s health services and women’s health outcomes, we collected a set of indicators for access to certain health services and health outcomes and created an index for each. 37 This analysis adopted a more holistic approach to women’s health, capturing gynaecological and maternal health indicators as well as measures such as healthy life expectancy and mental health services. In creating the indexes, we assessed each data set based on relevance, geographical coverage and granularity, temporal coverage, and overall quality. Each indicator was therefore deemed to be relevant to women’s health and potential inequality, covered all of England and was disaggregated at the upper tier local authority level (or could be apportioned to the upper tier local authority level), 38 had recent data to provide the most relevant picture of women’s health inequalities, and exhibited variation across localities.
We then assessed the interrelationship between the access and outcomes indexes with socioeconomic status and ethnic diversity. To understand the relationship between access and outcomes in conjunction with socioeconomic status, we assessed how the proportion of local authorities that rank higher than average in terms of access to women’s health services and health outcomes varies in terms of socioeconomic status, as measured by the index of multiple deprivation (IMD). IMD is scored on a scale of one to five and a lower IMD score represents greater levels of deprivation in each local authority. To understand the relationship between access and outcomes in conjunction with ethnic diversity, we assessed how the proportion of local authorities that rank higher than average in terms of access to women’s health services and health outcomes varies in terms of ethnic diversity.
Findings
According to the indicators selected and assessed, the analysis illustrated the following:
- Local authorities with higher ethnic diversity were found to have poorer access to women’s health services. 39 Figure 6 illustrates variation trends in the proportion of local authorities that rank higher than average in terms of access to health services as it relates to ethnic diversity. There is a clear negative correlation between women’s access to health services and ethnic diversity in local authorities. Among the top 20 per cent most diverse local authorities (fifth quintile), only 17 per cent score higher than average in terms of access to health services, compared to 83 per cent for the least diverse local authorities. This suggests that access is typically worse in the most diverse areas.
“I think there is a significant issue in access to diagnosis, specialist services and timely treatment to mitigate and minimise symptoms. I know in my situation I had to endure two failed coils before a thermal ablation was discussed at my request. The wasted years in my forties enduring two failed coils still makes me angry.”
- Analysis of the outcomes index by socioeconomic status reveals a strong relationship between more severe deprivation and worse health outcomes: local authorities with higher levels of deprivation experience worse health outcomes overall. For example, looking at just the local authorities with an IMD score of 5 (ie those in the top 20 per cent least deprived areas in the country), 97 per cent of them score higher in the health outcome index than the national average.
Chapter footnotes
- 7. Notably, these estimates do not account for other economic contributions, including business and property ownership, entrepreneurship and innovation, capital investment, volunteering, consumer spending, as well as education and skill development. ↑
- 8. From April 2020, interviewers were advised to assign coronavirus to ‘other’. ↑
- 9. Totals may not amount to 100 due to rounding. ↑
- 10. Additional methodology details can be found in the Appendix. ↑
- 11. The BCS tracks the lives of approximately 17,000 individuals who were born in the UK in a single week in 1970, and this cohort has been surveyed nine times since the original survey (at birth), with the latest wave being conducted at ages 46-48. The RHS collected data from approximately 60,000 individuals across England in Autumn 2023. Refer to the Appendix for more information on these data sources. ↑
- 12. During this analysis of the BCS, primary dysmenorrhea is defined as experiencing either heavy periods (ie menorrhagia) or painful periods, and not having an underlying diagnosis of endometriosis, fibroids or ovarian cysts. ↑
- 13. Given the limitations of the questions asked in the BCS, for the purposes of this study, secondary dysmenorrhea includes experiencing either heavy or painful periods as well as having a diagnosis of endometriosis, fibroids (myomas) or ovarian cysts. This is not an exhaustive assessment, as secondary dysmenorrhea can additionally encompass adenomyosis, endometrial polyps, and pelvic inflammatory disease. ↑
- 14. As the survey is conducted via self-reporting symptoms, which can occur throughout both perimenopause and menopause, this assessment is inclusive of both perimenopausal and menopausal individuals. ↑
- 15. As noted in the ‘Language’ section of this report, we do not intend to classify the perimenopause or menopause as a ‘condition’ or ‘disease’ as it is indeed a physiological process that most people assigned female at birth will experience. Rather, we use this term to maintain consistency with our data sources and underscore the impact that the effects of more severe perimenopause and/or menopause can pose to individuals. ↑
- 16. A dummy variable is one that takes a binary value, either 0 or 1, to indicate the outcome. In this instance, the variable takes the value of 1 if the respondent is in employment, and 0 otherwise. ↑
- 17. According to the UK’s largest employee wellbeing survey (2024), employers lost 20 per cent of working hours due to presenteeism in 2023, amounting to a loss of 49.7 productive days per employee per year. ↑
- 18. These values are not mutually exclusive impacts due to data formatting. For example, a high proportion of those that experience painful periods also stated that they experience heavy periods. Due to the survey structure, it is not possible to estimate the relative sizes of the impact of heavy periods, painful periods, fibroids, ovarian cysts, and/or endometriosis on absenteeism and presenteeism given the substantial overlap between these groups. ↑
- 19. A percentage point refers to the absolute difference between two percentages. For example, if 30 per cent of women who do not experience dysmenorrhea were miserable or depressed, and experiencing primary dysmenorrhea is associated with a 7 percentage point increase in the likelihood of being miserable or depressed, this would imply that 37 per cent of women experiencing primary dysmenorrhea are miserable or depressed. ↑
- 20. This number does not capture the approximate 5 per cent of the population who enter the menopause prematurely due to certain cancer treatments, surgery, or certain health conditions. ↑
- 21. For the purpose of the analysis, we proxy ‘less severe’ and ‘more severe’ based on the number of symptoms the woman is experiencing. Though we recognise this does not account for the ‘severity’ of the individual symptom (eg how often and how debilitating the symptoms are), this is a proxy based on the data available. ↑
- 22. joint aches and pains, hot flushes, cold/night sweats and vaginal dryness. The treatment group is split into those that reported that they experience 1-2 of these symptoms and those that experience 3-4 symptoms, as a proxy for the severity of the condition. ↑
- 23. The eight menopause symptoms accounted for in the RHS include including difficulty sleeping, low mood or anxiety, hot flushes, night sweats, vaginal dryness, discomfort during sex, reduced sex drive, and problems with memory or concentration. ↑
- 24. Median pay for women of menopausal age was calculated using ONS data on earnings. Earnings data by age is only published in wide age bands, so an average of the median take home pay within the 40-49 and 50-59 age brackets is used. This is a weighted average, adjusted by the number of females in employment across the two groups. This results in a median annual gross pay for women of menopausal age of £23,900. ↑
- 25. Siloed commissioning structures detract from holistic care provision and undermine health outcomes. For instance, polycystic ovary system (PCOS) – an endocrine disorder which can contribute to infertility, cardiovascular disease, pregnancy complications, non-alcoholic fatty liver disease, and endometrial cancer – will not be adequately accounted for in this proxy. Moreover, specialities such as vulval dermatology that manage lichen sclerosis, vulval psoriasis and recurrent thrush will not be accounted for in this proxy. Thus, while obstetrics and gynaecology services comprise a sensible evidence base for investigation, it will not account for the multifaceted and multi-system impact of women’s health. ↑
- 26. For instance, contraception is frequently used as a first-line treatment for menstrual health problems. Notably, there is compelling evidence (Public Health England, 2018) surrounding the ROI of publicly funded contraception in England, indicating a £9.00 saving for every £1 invested in publicly provided contraception. ↑
- 27. Additional methodology details can be found in the Appendix. ↑
- 28. Staff in obstetrics and gynaecology is defined as the FTE in ‘Obstetrics & gynaecology’ in the Medical Staff table by CCG of NHS England. Staff in maternity services is defined as the FTE in ‘Maternity Services’ in the Non-Medical Staff table by CCG of NHS England. All three staff categories – obstetrics, gynaecology, and maternity – are included in this proxy. ↑
- 29. The analysis investigates the variation in investment in obstetrics and gynaecology services across different clinical commissioning groups (CCGs) over two consecutive tax years and assesses the impact on economic performance indicators over the subsequent three tax years. ↑
- 30. Gross value added per head, for both the female and male population, is used to capture spillover effects that investment in women’s health can have on the wider population. ↑
- 31. While NHS sickness absence data disaggregated by sex at the required geographical granularity is not available, women represent approximately three-quarters of the NHS workforce (NHS workforce statistics). As such, the use of overall NHS sickness absence is appropriate. Sickness absence rate is calculated by dividing the sum total sickness absence days (including non-working days) by the sum total days available per month for each member of staff (NHS Workforce Statistics, 2024). ↑
- 32. While the main changes to NHS systems occurred following 2019, there were select mergers and splits in certain CCGs’ geographies, which could have introduced data errors due to geographical apportioning. These CCGs were therefore excluded from the analysis. Of the 211 CCGs for the 2014/15 tax year, we assessed 176 (83 per cent). ↑
- 33. Primary care was not included in this analysis given the lack of clear data surrounding primary care staff members performing obstetric and gynaecological activities (ie GP with specialist interest). During the validation process of the proxy, we tested an alternative formulation that included primary care expenditure. However, this approach showed poorer alignment with the data obtained from a selection of integrated care boards (ICBs). Having assessed select coding data in primary care and discussed women’s health in the context of primary care with several general practitioners, we understand that repeat presentations in primary care have been compounding capacity issues and driving up costs to providers, indicating that while women’s health expenditure in primary care settings may not vary across systems, it is a necessary pillar of delivering women’s health services and will be a critical part of the solution. ↑
- 34. A CCG was classified as a high investor for a specific period if it belonged to the top 33 per cent of the distribution of changes in NHS expenditure in obstetrics and gynaecology services relative to need during that period. Similarly, it was classified as a low investor if it fell into the bottom 33 per cent of the distribution. ↑
- 35. As outlined in the longitudinal analysis, this matching process ensured that the comparison between high and low investors was made between CCGs with similar baseline characteristics, thereby providing a more accurate estimate of the impact of investment levels in obstetrics and gynaecology services, barring key confounding factors. ↑
- 36. Additional methodology details can be found in the Appendix. ↑
- 37. The data underpinning the analysis can be found in the Appendix. ↑
- 38. ONS data on sickness absences was available only at the regional level. It was therefore necessary to apportion this data to the upper tier local authority level using population data. The lower quality of this specific indicator is reflected in the weighting strategy of the index. That is, sickness absences are given a slightly lower weighting than other indicators due to the need to apportion the data. ↑
- 39. This data does not fully capture the barriers to access faced by those subject to ‘No Resource to Public Funds’ conditions, those with insecure migration status, those from the Romani, Roma, and Irish Traveller communities, or those who may need to access an interpreter during their service. ↑
Conclusion
This report has evidenced the impact that certain women’s health conditions, if left neglected, can pose to the economy; the benefits of boosted investment across obstetrics gynaecology services; and the variation in women’s health service access and outcomes based on ethnic diversity and deprivation across local authorities. Our intention is to showcase the extent of the gender health gap as it relates to the economy; the potential ROI of further investment; as well as the underlying notion that investment alone will not close the gender health gap. In tandem, we must grapple with the sexist and racist roots upon which modern medicine was founded, interrogating why – despite longstanding plans and policies – certain services continue to decline, and inequalities proceed to widen. Thus, we call for investment in women’s health that promotes sustainable, inclusive growth, ultimately contributing to both an economy and a health system that work better for everyone.
Despite this report’s focus on the relationship between women’s health and economic growth, and the undeniable economic benefits that further investment in women’s health pose, the case for further investment in women’s health is not just about the economy. Health impacts every element of our lives, and access to equitable healthcare that is of appropriate quality and provided without bias or discrimination is a human right that should be protected and guaranteed regardless of the economic benefits it poses to society. While we have made a ROI case, at the heart of this evidence is a view that women have a right to a good quality of life that allows them to participate fully and equally in society.
Recommendations
His Majesty’s Treasury (HMT)
In its manifesto, the Labour Party said: ‘Never again will women’s health be neglected. Labour will prioritise women’s health as we reform the NHS.’ Prioritising women’s health will require resource as well as a comprehensive understanding of where funding is needed most. Investing in women’s health falls naturally into Labour’s growth agenda, more pointedly under the pillars of investment and reform. As such, we recommend that HMT:
- allocates ringfenced and long-term funding for the remaining eight years of the Women’s Health Strategy for England, explicitly recognising the role that better health for all, and specifically those who face inequalities, can play in terms of NHS savings, labour market participation, and wider prosperity
- allocates additional funding to the National Institute for Health and Care Research for women’s health research to promote understanding of and treatment options for conditions that solely affect women as well as those that affect women differently or disproportionately
- works alongside the Department of Health and Social Care to ensure that established women’s health hubs have the financial support necessary until the anticipated return on investment is realised.
Department of Health and Social Care (DHSC)
- Additional funding for the women’s health hubs should be allocated according to population needs across the 42 integrated care systems (ICSs), proportionate to costs and ringfenced to allow for the economic benefits of their implementation to be recognised.
- Combined authorities and mayoralties should have an explicit responsibility and dedicated funding to coordinate with ICSs and local authorities to join up sexual and reproductive health services, making the process for patients more streamlined, and commissioning roadblocks less obstructive than they currently are.
- Prior to creating any new policies or plans, the Secretary of State for Health and Social Care should work with the minister for women’s health and the women’s health ambassador to interrogate why existing ones have fallen short. They should outline how they will close the black and Asian maternal mortality gap, as outlined in Labour’s manifesto, and commit to a plan that addresses disparities in outcomes based on race, ethnicity, and deprivation.
- Given a deputy women’s health ambassador was announced but never appointed, we recommend that the DHSC prioritise filling this role with an ambassador for women’s health focused specifically on improving outcomes for black, Asian, and minority ethnic women.
- Encourage women’s health hubs to be centres for more robust data collection, research, and more innovative technologies such as advanced ultrasound diagnostic facilities to aid accurate and timely diagnoses. Funding should be made available for recruitment and upskilling of staff to conduct ultrasound scans effectively.
- At the heart of any emerging policies and plans – including the NHS ten-year plan – should be an explicit equity agenda as well as proportionate funding to support implementation.
- Work alongside the Department for Work and Pensions (DWP) to develop more advice and information for employers surrounding women’s health conditions, such as reasonable adjustment policies or the provision of period products in toilets.
NHS England (NHSE)
- Any future NHS workforce plans should overtly recognise the pivotal role that women – alongside their health – play in the NHS workforce and be explicit about ways in which women’s health will be supported.
- Lead the creation of a women’s health data repository that houses information surrounding key metrics including condition prevalence, diagnostics, and ICS expenditure data, with the aim of making women’s health data more readily available for research and innovation. Data should be disaggregated by the distinguishing characteristics that impact the care that women receive as well as the outcomes that they experience, including but not limited to sex, gender, race, ethnicity, sexual identity, sexual orientation, disability, education, income level, and age.
- Reconsider the way in which gynaecology is prioritised with a focus on the wider impacts on patients waiting for care. Elective recovery should address the unequal growth of gynaecology waiting lists when compared to other specialties. Appropriate staffing levels should be established to prioritise gynaecology services in a safe and effective way.
- Collaborate with the General Medical Council (GMC) and the National Institute for Health and Care Excellence (NICE) to refurbish training and guidelines for health and social care professionals – including medical students – surrounding women’s health needs, encompassing cultural sensitivities, trauma-informed approaches and the overarching importance of listening to women and taking reported symptoms, such as pain, seriously.
National Institute for Health and Care Research (NIHR)
The NIHR’s introduction of a ‘challenge’ to tackle maternal inequalities alongside its newly founded Policy Research Unit on Reproductive Health are welcome advances for women’s health research. However, given research into reproductive and maternal health have hovered stagnantly around 2 per cent of total public research funding over the past decades, much more investment is needed. Moreover, as evidenced throughout this report, there is a need for more research into conditions that affect both men and women albeit differently or disproportionately, but the NIHR does not publish data on the amount of funding that is allocated to understanding how these conditions manifest differently.
As such, we recommend that the NIHR:
- commits to tackling gender bias in research by ensuring that women are adequately represented in clinical trials and improving data collection disaggregated not only by sex and age, but also gender, race, ethnicity, sexual identity, sexual orientation, disability, education, and income level
- commits to a year-on-year 1 per cent increase in overall public research funding that is dedicated to ‘reproductive health and childbirth’, disaggregating the funding allocations to illustrate the total award allocated to maternity versus gynaecology services
- prioritises research surrounding conditions that affect women differently or disproportionately, such as autoimmune diseases, rheumatoid arthritis, osteoporosis, cardiovascular disease, and dementia and publish data delineating the amount of public funding allocated for this research
- prioritises research into innovative diagnostic and treatment options for women’s health conditions that prioritise early diagnosis and intervention alongside minimal invasiveness
encourages further research in the field of women’s health economics, including critical topics such as infertility and cardiovascular disease.
Office for National Statistics (ONS)
When collecting data on economic activity and labour market participation as they relate to health, include gynaecological health such as the menopause or menstruation to allow for a better understanding of the extent to which gynaecological health can impact women’s ability to participate in the workforce.



