Key points
Extra NHS appointments alone will not be enough to solve the NHS waiting list crisis. The new Labour government has pledged to ensure 92 per cent of patients wait no longer than 18 weeks from referral to treatment (RTT) – a target that has not been hit for nearly decade – by delivering an extra 40,000 NHS appointments, operations and diagnostics every week, equivalent to 2 million a year.
There are currently over 7.5 million unresolved open care pathways, impacting an estimated 6.4 million individuals in England. Nearly 4 million of these unresolved open pathways are part of a significant backlog that has accumulated over the last decade.
To meet and sustain the 18-week standard, two fundamental objectives must be achieved simultaneously:
The NHS must provide enough consistent care to achieve the 18-week standard annually, recognising the growing and ageing population, increasing complexity of cases and continuous adoption of innovation.
The additional backlog that exists must be tackled through additional treatments. The additional capacity required to achieve this should be viewed as a one-off requirement.
Treatment often requires a combination of outpatient, diagnostics and inpatient care (through day-case procedures and overnight stays). On average a pathway of care that does not require an admission to hospital includes 1.4 outpatient appointments. Twenty per cent of people go on to an admission which typically requires a further 0.9 outpatient appointments and a hospital admission, 80 per cent of which are day cases and 20 per cent involve an overnight stay. Diagnostics form a significant element of the pathway but are not considered in this report due to constraints in access to diagnostics data at healthcare specialty level.
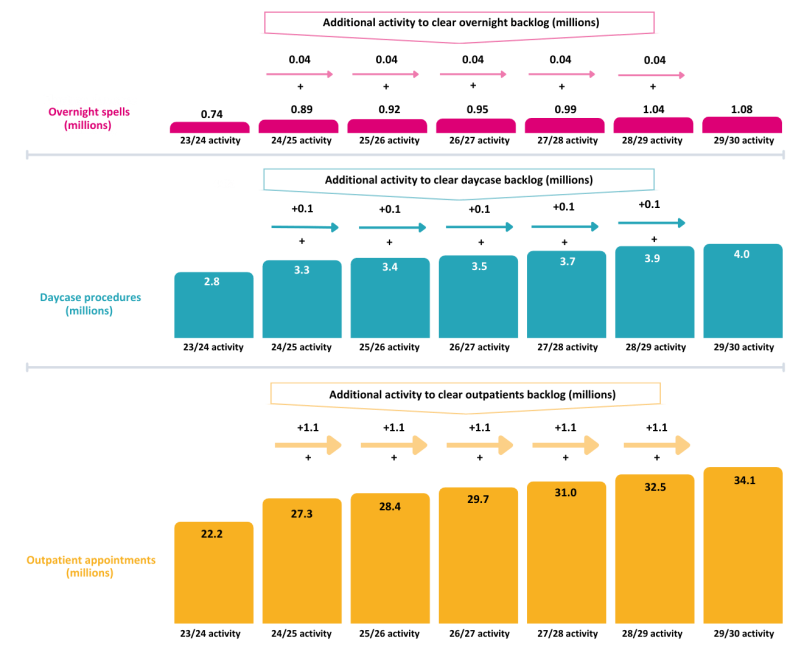
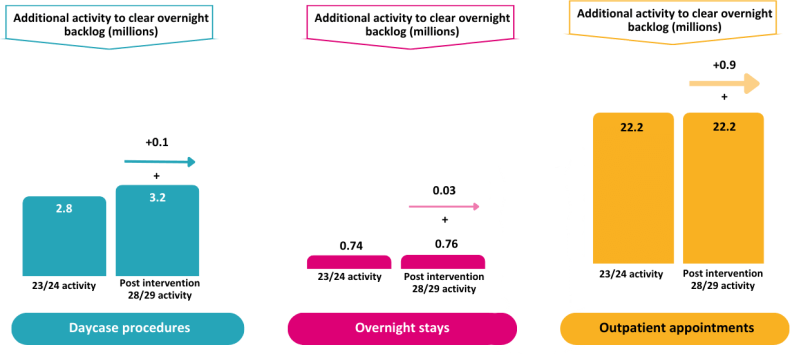
Treating sufficient referrals to maintain the business as usual (BAU) waiting list in 2024/25 – in line with the 18-week standard – requires 27.3 million outpatient appointments, 3.3 million day-case procedures, and 890,000 overnight stays. In 2023/24, the NHS completed 22.2 million outpatient appointments, 2.8 million day-case procedures, and 740,000 overnight stays related to RTT pathways, when industrial action is accounted for. Consequently, without transformation, an additional 5.1 million outpatient appointments, 0.5 million day-case procedures and 150,000 overnight stays are needed this year, simply to prevent the waiting list from increasing further.
Achieving and sustaining the 18-week standard also means planning for increased future demand. The historic trend is that this demand grows in aggregate at 3.8 per cent per year – noting there is significant geographical and healthcare speciality variation that needs to be considered.
Based on current levels of growth in the need for care and how care is currently delivered, this means that, by 2028/29 the NHS will need to do 50 per cent more elective activity than it is currently doing to clear the wait list and sustain achievement of 18-week performance. Without being accompanied by change and reform, the government’s promise of an extra 2 million appointments, operations and diagnostics a year addresses about 15 per cent of the additional requirement.
A more transformational response is required to ensure the public can be confident the NHS can offer timely access to elective care. Change is needed in every step of the pathway of care: it requires both a strengthened and renewed focus on existing initiatives as well as a more radical approach to the creation of elective hubs and centres of expertise for complex care. Taking each step of the pathway in turn, the required elements of the response are as follows:
Assessing the drivers for rising demand for elective treatment, and ensuring people are receiving the right care: by preventative interventions that reduce the need for care in the first place as well as streamlining the referral process between GPs and specialists, and ensuring people living in deprivation have equal access to services.
Digitalising waiting-list management and continuously validating the patient tracking list: embracing tools available as part of Federated Data Platform more widely to improve efficiency and accuracy and supporting staff to adopt digitally-enabled management practices for the elective pathway.
Transformation of outpatient elective care for people who do not need a hospital admission: through more integrated, holistic care, involving fewer appointments and resources for people with more than one open care pathway; standardising care with defined best practice pathways considering each speciality and different patient needs; the adoption of the latest technology and innovation to transform outpatient care, including process automation, the application of artificial intelligence and robotics.
Creating elective hubs for people whose treatment involves an admission to hospital: initiating an accelerated development programme to almost double the current dedicated elective hub capacity on sites without emergency activity – an approach already proven to work – providing quicker access and ringfencing planned care resources. Capital funding with streamlined decision-making will be essential to facilitate this.
Creating centres of expertise for complex elective admitted care: combining this approach with optimal use of elective hubs creates capacity on ‘hot’ sites, both to decompress them from high occupancy levels enabling better care for emergency patients, and to provide capacity for complex planned care that needs to be co-located with the other services on major hospitals. Capital to remodel the existing hospital estate, making it fit for modern practice, will again be essential.
Focusing on the enablers of change critical to transforming care: long-term aligned planning is needed that brings together capital investment; pathway-based funding; workforce planning linked to demand; fostering clinical leadership and accountability; high-quality booking and scheduling; continuous improvement of data quality and widespread adoption of digital innovations; and staff, including team-based training and development to enhance improvement capabilities.
Addressing the residual backlog of patients waiting: acting on points two and three, alongside early implementation of points four and five with the capacity needed for 2029/30 put in place by April 2026 would address much of the excess numbers of people waiting. However, more would still be needed. To address this, a combined approach is needed, including incentivising NHS staff to work out of hours, using insourcing providers to make additional use of NHS capacity out of hours and outsourcing activity to private healthcare providers.
If all of the opportunities in this report were implemented together, the government’s early promise of an additional 2 million appointments, operations and diagnostics a year would deliver the additional requirement. While improvements are underway across the country, major transformation is required in the way care is planned and delivered, with significant investment, energy and government commitment to make it happen.

Introduction
More people are currently waiting for NHS planned care than ever before. The new Labour government paves the way for a fresh approach to tackling this crisis, with the party promising “an extra 40,000 NHS operations, scans and appointments every week, equivalent to two million a year”. This will be achieved through enabling neighbouring hospitals to share waiting lists, commissioning the independent sector to supply additional capacity, and incentivising staff to work out of hours. But are these steps enough to ensure the 18-week standard for completing elective care is met and sustained?
Labour’s pledge to uphold constitutional standards is commendable, and the additional 2 million appointments a year is a promising start. However, this alone will not suffice to ensure people consistently receive care within 18 weeks. To achieve the standard, 92 per cent of people should begin treatment within 18-weeks – whether that is starting medication or having a procedure. Given that the NHS has struggled to meet this standard for over a decade, a more sustainable plan and transformative approach is necessary. Now, with the new government developing a ten-year plan for the NHS, there is an opportunity for bold and decisive action. This paper outlines what the NHS can do to reliably and confidently achieve the 18-week standard for the benefit of the population.
The imperative for action is clear. Long periods of time spent waiting for treatment have widespread implications for people and their families across the country. Consequently, waiting times are a leading cause of public dissatisfaction with the NHS. Long waits lead to worse patient outcomes; for instance, when surveyed on this issue, 40 per cent of patients consider their condition to have worsened in the time between referral and admission, and 57 per cent said it affected their wellbeing.
It is important to contextualise upfront that the increased waiting lists are not caused by inherent inefficiency within the NHS. All things considered, the NHS is treating more people than ever before, on an emergency and planned basis, and the care that it delivers is more complex than it ever has been, too.
Nevertheless, the latest figures show there are 7.6 million care pathways that are currently open and have not been resolved through treatment. The 7.6 million care pathways are for 6.4 million individuals (i.e. some individuals have more than one care pathway open), with more people than ever waiting longer than a year for their treatment. These figures will continue to grow over the long term, until additional steps are taken to ensure services have planned for the changing and growing needs of the population, and have the resilience and capacity required to meet this need.
The 18-week standard and how it should be achieved in theory
Each year, individuals present with health concerns that require planned specialist-led care. This is referred to this as ‘business as usual’ demand, or BAU for short. Meeting the 18-week standard means the NHS should have sufficient capacity to treat each referred individual within 18 weeks, in line with NHS referral to treatment (RTT) rules, set out in the NHS Constitution. These rules have been in place since 2004. The number of people joining and leaving the waitlist, known as the patient tracking list (PTL), should be balanced, ensuring a consistent and defined number of individuals wait no more than 18 weeks. This prevents the waitlist from increasing over time, causing a backlog.
The challenges in achieving the 18-week standard
Unfortunately, achieving the 18-week standard has been a challenge for quite some time. The size of the NHS waiting list dropped to its lowest point in 2009/10 and held roughly flat until 2012/13. By 2019/20 (pre pandemic), it had grown by 75 per cent. It then proceeded to increase by a further 75 per cent until 2023/24 (post pandemic) – see Figure 1.
Figure 1: The total number of open care pathways across all providers over the past ten years

Source: NHS Referral-to-Treatment Statistics, CF analysis.
The number of people joining the patient tracking list has been consistently higher than the number of people receiving treatment since new referral records began (in October 2015) – see Figure 2.
Figure 2: Numbers joining the PTL as compared to the numbers leaving the PTL from October 2015 to April 2024
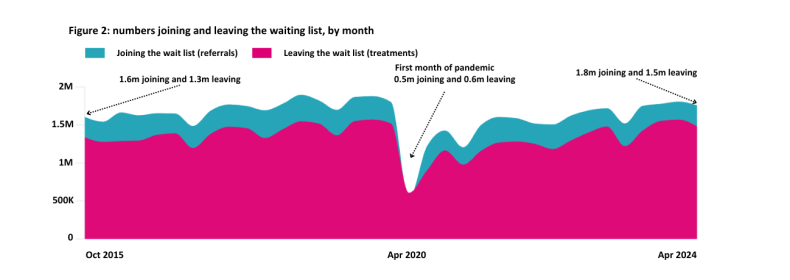
Source: NHS Referral-to-Treatment Statistics, CF analysis.
Undoubtedly, the growth in the waiting list is partly related to demographic change, with an increasing amount of the population living in older age and therefore requiring more planned care to manage long-term conditions. This is evidenced by the rise in the number of people who are referred to treatment each year and who join the waiting list. In England this has increased from 18.9 million in 2016/17 to 20.5 million in 2023/24. Since 2022/23, the growth rate has been 3.8 per cent per year.
The rise in the need for care applies also to urgent and emergency care. Unplanned care has risen by 10 per cent since 2015/16, and last year the NHS handled 5.4 million emergency admissions compared to 4.9 million in 2015/16. The way services are organised on most acute hospital sites means capacity, particularly beds, can be diverted to emergency care. Over time this has a knock-on impact on the amount of elective care that takes place – see
Figure 3.
Figure 3: Change in episode volumes by point of delivery between 2015/16 and 2022/23
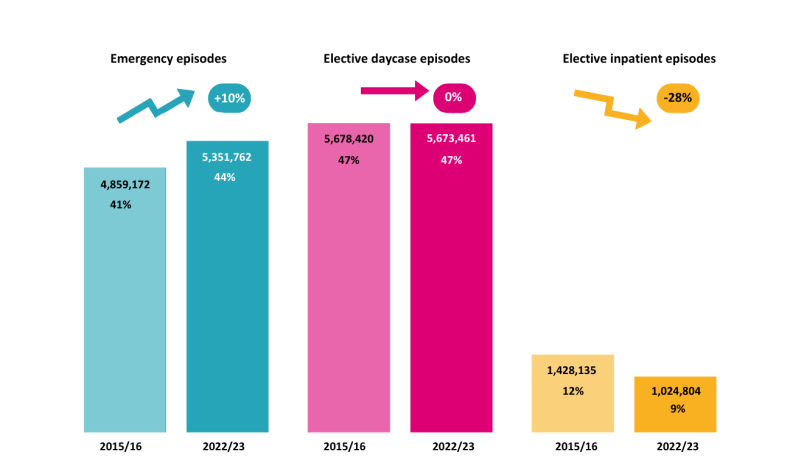
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, CF analysis.
This phenomenon has also caused a long-standing drop in elective care activity over winter – see Figure 4. Latest operational guidance advises annual average bed occupancy levels of 92 per cent. However, the profile of emergency activity across a year means that during winter months many hospital providing emergency care have bed requirements that exceed 100 per cent. This results in pauses or delays to elective care – an issue highlighted by the Royal College of Surgeons.⁸
Figure 4: Change in activity levels over winter from 2018/19 to 2023/24
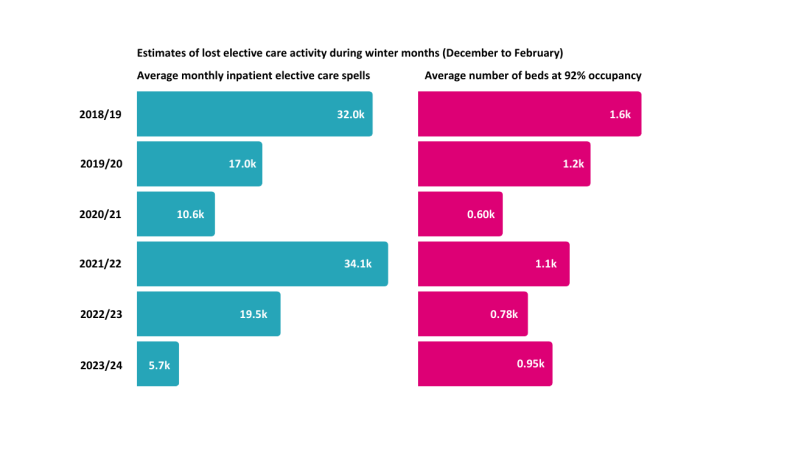
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, CF analysis.
The combination of demographic change and delaying planned care has resulted in steadily increasing complexity in both elective and emergency care over the past three years – see Figure 5.
Figure 5: Complexity index for emergency and planned care over time
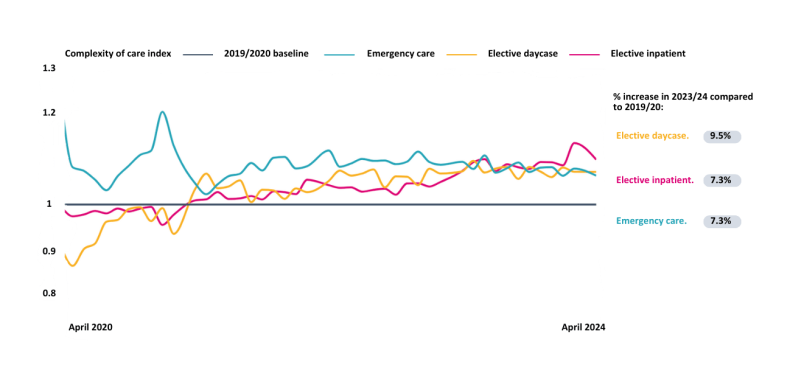
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, 2019/20 National Tariff Payment System, CF analysis.
The management of the COVID-19 pandemic only exacerbated these existing issues. A series of successive pauses in elective care enabled staff and beds to be freed up to deal with the management of the pandemic. This resulted in a 73 per cent increase in the number of open care pathways – from 4.4 million in March 2020 to 7.5 million in March 2024 – with median wait times rising from just under nine weeks to nearly 15 weeks over that same period. The number of care pathways that were open for longer than the 18-week standard also rose from 860,000 to 3.2 million, a fourfold increase, and those open longer than a year rose from 3,000 to 309,000, a 100-fold increase – see Figure 6.
Figure 6: Proportion of care pathways open for longer than 18 weeks and 52 weeks over the last 15 years
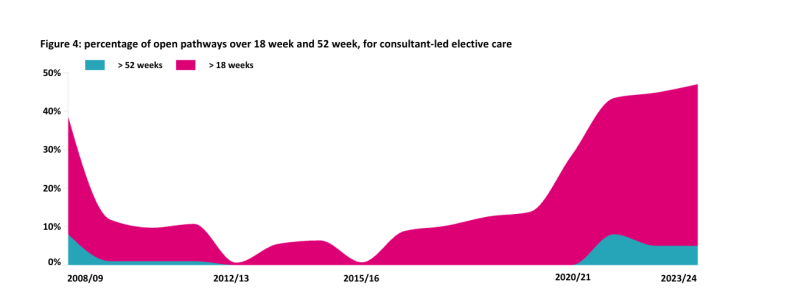
Source: NHS Referral-to-Treatment Statistics, CF analysis.
In more recent years, industrial action across NHS staff has also had an impact on planned care delivery, with procedures being delayed. In 2023/24, industrial action by doctors took place on 41 days. While this had no impact on outpatients and a small impact on day-care procedures, elective inpatient care suffered. On average, days with industrial action had 25 per cent fewer overnight procedures completed, with in total 45,500 day-case procedures and 29,700 overnight procedures being lost in 2023/24 – see Figure 7.
Figure 7: Change in activity levels on days with industrial action compared to days with no industrial action in 2023/24
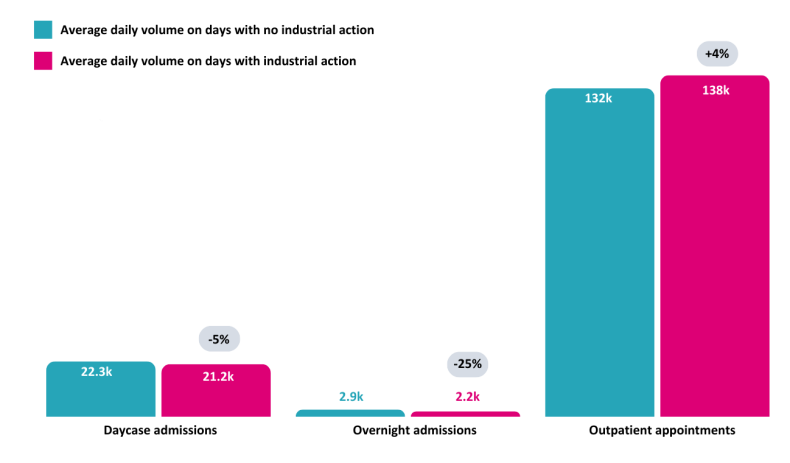
Source: NHS Referral-to-Treatment Statistics, CF analysis.
The combined result is that the RTT standards have not been met for many years, and the last time the overall 18-week standard was met was in February 2016. Despite numerous initiatives and requirements for improvements, as outlined in NHS England’s Priorities and Operational Planning Guidance, the main issue persists: there are more people joining the waiting list than leaving it.
Achieving the 18-week standard also means planning for increased demands in the future. The burden of ill health and consequent demands on the NHS will continue to increase, as the size of the UK population aged 65 years and over is projected to increase from 13 million (19 per cent of the population) to 16.5 million (25 per cent of the population) over the next 15 years. This will result in an associated increase in frailty and long-term conditions, with research from The Health Foundation estimating that 9.1 million people in England will be living with major illness by 2040, an increase of 2.5 million people compared to 2019.
Why current plans do not reach far enough
To get to a position where the NHS can meet and sustain the 18-week standard, two fundamental objectives must be achieved:
- The NHS must provide enough consistent care to achieve the 18-week standard annually, recognising the growing and ageing population, the increasing complexity of cases, and the continuous adoption of innovations.
- The additional backlog that exists – due to insufficient treatments taking place over the past decade, as well as pauses in elective care during the pandemic – must be tackled through additional treatments. The additional capacity required to achieve this should be viewed as a one-off requirement.
To address point one, in 2024/25, 3.6 million referrals should be managed at any one time to respond to the expected need for care. This is the BAU waiting list size – as it is the size the waitlist should be to achieve the 18-week standard.
For the people on the waiting list, treatment often requires more than one contact with the NHS, and a combination of outpatient, diagnostics and inpatient care (through day-case procedures and overnight stays) – see Figure 8 on the following page. Diagnostics form a significant element of the pathway but are not considered in this report due to constraints in access to diagnostics data at healthcare specialty level.
Figure 8: The current pathway for people needing planned care
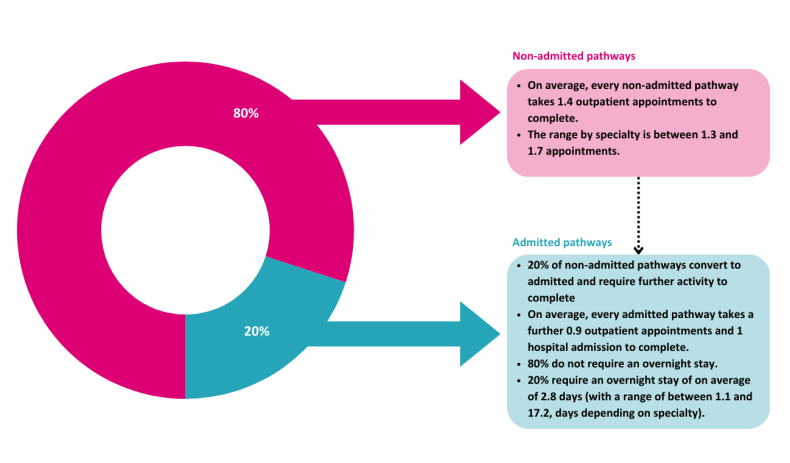
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, CF analysis.
With this in mind, treating sufficient referrals to maintain the BAU waiting list in 2024/25 – in line with the 18-week standard – would require 27.3 million outpatient appointments, 3.3 million day-case procedures, and 890,000 overnight stays. As a comparison, in 2023/24, the NHS completed 22.2 million outpatient appointments, 2.8 million day-case procedures, and 740,000 overnight stays related to RTT pathways, when industrial action is accounted for. In other words, without transformation, there would need to be an additional 5.1 million outpatient appointments, 0.5 million day-case procedures and 150,00 overnight stays occurring this year, simply to prevent the waiting list from increasing further – see Figure 9 on the following page.
Figure 9: The additional activity required to meet the BAU elective care demand in 2024/25
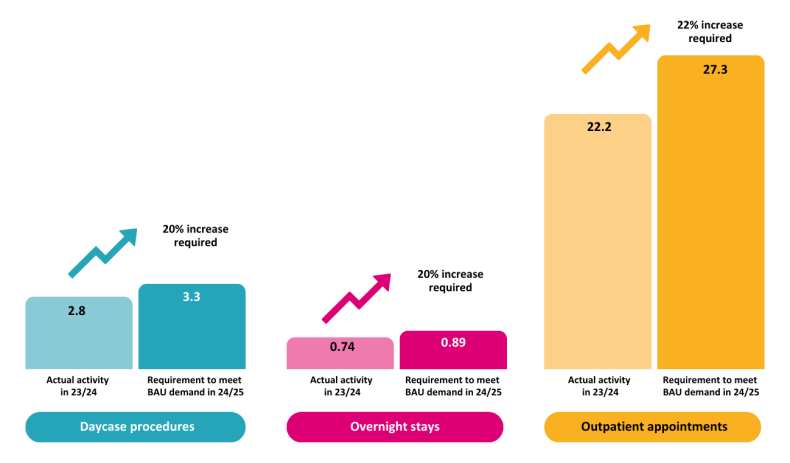
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis.
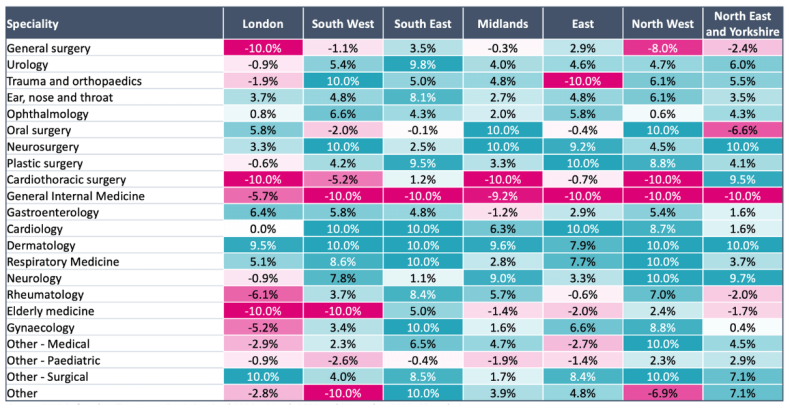
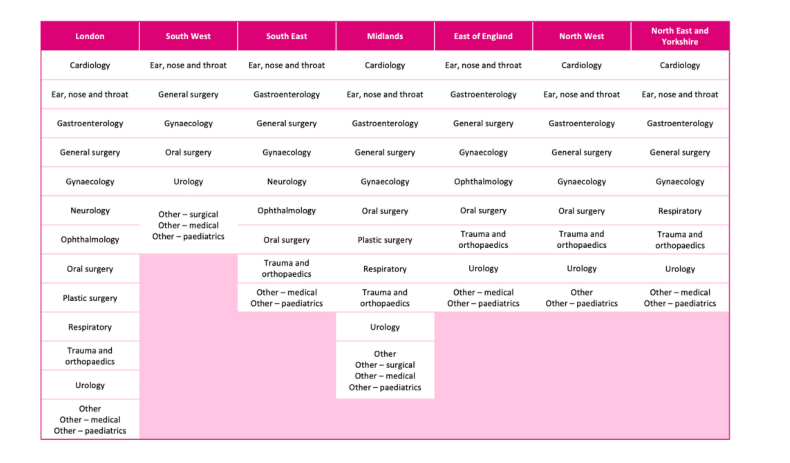
It should be noted that there are no agreed optimal care pathways for different healthcare specialties. While some variation in pathways is to be expected due to the different requirements of individual patients and conditions, the level of variation is unexplainable – see Figure 10 on the following page. More standardised pathways should be defined at specialty level, embedding consistent best practice (defined best practice pathways should also inform payment to providers – more on this later).
Figure 10: Variation in activity per referral (‘clock start’) by health specialty and region
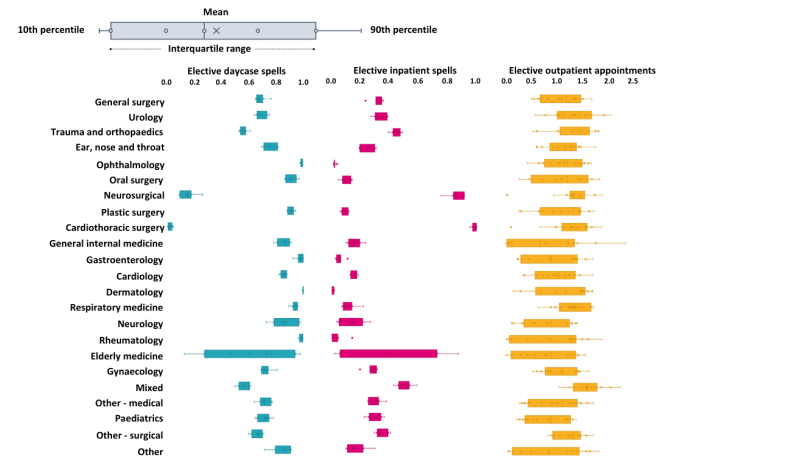
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, CF analysis.
Based on current trends, the number of people joining the BAU waiting list is also expected to rise by 3.8 per cent every year for the next five years, due to population growth and underlying changes in demand for planned care. 3.8 per cent is the aggregate change in demand, however, at a healthcare specialty level there is wide variation from -18 per cent for general medicine to +11.4 per cent for dermatology – see Figure 11* on the following page. 1 There is also wide variation geographically from 0.5 per cent in London to 8.2 per cent in the South East. 2 To consistently and sustainably achieve the 18-week standard, the specific growth rates for healthcare specialities and the population in question need to be planned for.
Figure 11: Expected growth rates for referrals to care pathways based on historic growth for the next five years (2024/25 – 2029/30)
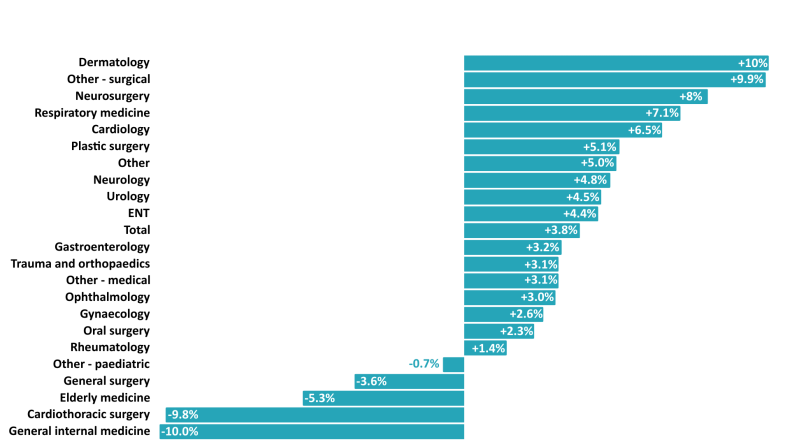
Source: NHS Referral-to-Treatment Statistics, CF analysis.
Assuming the need for care continues to grow in the ways observed and there is no change in the way care is delivered, by 2028/29, the NHS should be providing 32.5 million outpatient appointments (10.3 million more than 2023/24), 3.9 million day-case procedures (1.1 million more), and 1 million overnight stays (300,000 more) per year. This is simply to meet BAU demand with the projected increase in demand due to population growth and changing demographic profile. In short, activity will need to increase by 46 per cent over the next five years to effectively meet BAU demand for elective care.
In addition to managing the BAU workload and its expected growth, the NHS will need to treat an additional 3.96 million people who are currently on existing wait lists to address the one-off requirement of the backlog of people waiting. Spreading this one-off requirement over the five years would take an additional 1.1 million outpatient appointments, 120,000 day-case procedures and 36,000 overnight stays, per year. 3
Putting all of this together, in 2028/29 the NHS would need to do 33.6 million outpatient appointments, 4 million day-case procedures and 1.1 million overnight stays – equivalent to 50 per cent more activity than it is currently doing in total – see Figure 12. This would clear the wait list back to levels that would sustain 18-week performance.
This highlights the transformation required to achieve the standard. Without being accompanied by change and reform, the government’s early promise of an additional 2 million appointments, operations and diagnostics a year addresses about 15 per cent of the additional requirement.
Figure 12: BAU activity and additional required to clear elective care backlog in five years
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis.
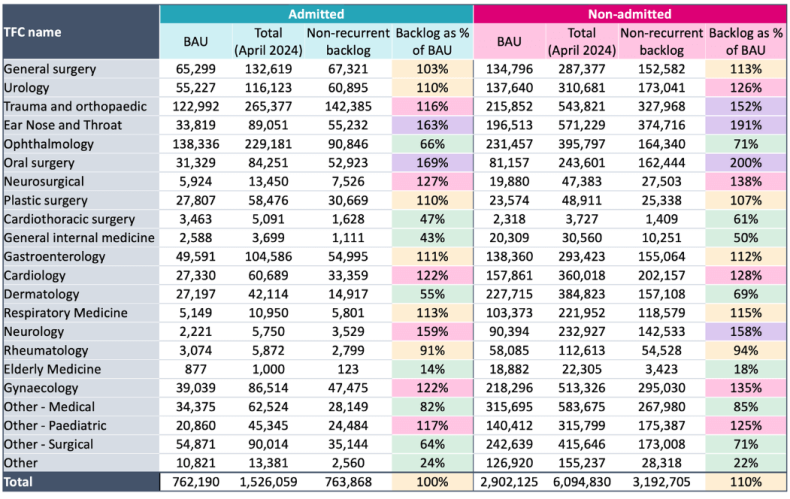
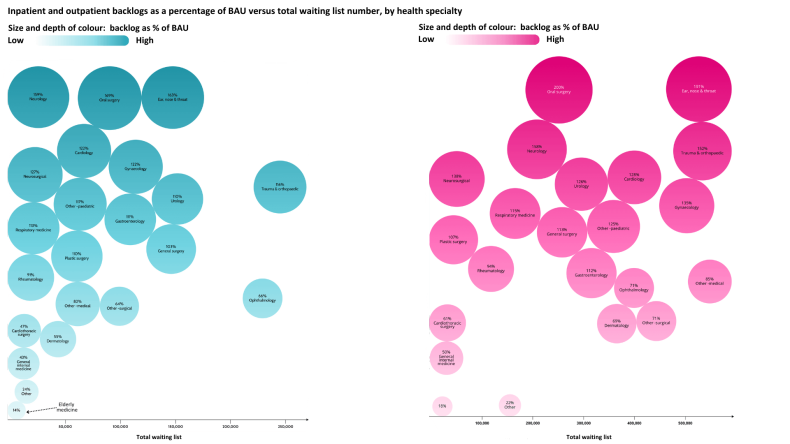
The requirement is not equal by service type: some healthcare specialties have a much bigger challenge to deliver BAU requirements than others and therefore will experience greater difficulties in tackling backlogs – see Figure 13, where the non-recurrent backlog for each specialty has been separated and expressed as a percentage of the BAU waiting list to demonstrate this point.
Figure 13: Non-recurrent backlog for inpatient and outpatient care, expressed as percentage of the BAU inpatient waiting list for March 2024
Source: NHS Referral-to-Treatment Statistics, CF analysis.
Chapter footnotes
Priority actions needed to deliver elective recovery in five years
To address this large shortfall over the term of the government, care needs to become more efficient, with a reduction in the amount of activity required to deliver pathways, so that treatments conclude with fewer resources. In addition, the overall amount of activity that takes place needs to rapidly increase.
Much has been tried already with incremental requirements to improve, with a particular focus on people waiting a very long time. Various initiatives have been tested and implemented through NHS England’s Elective Recovery Plan and the Operational Planning Guidance, but the focus on 65 and 52-week waits has created distortion in how organisations address the elective recovery challenge.
Although elective recovery is a clear priority for the government, a holistic plan and a more transformational approach is needed, incorporating proven innovations and best practices to meet and sustain the 18-week standard. The remainder of this report focuses on the actions needed to sustainably deliver the 18-week standard and address the one-off requirement to treat the excess number of people waiting now. It covers:
- The drivers of rising demand for elective care, and ensuring people are receiving the right care.
- Digitalising waiting-list management and continuously validating the PTL.
- Transforming outpatient care, for people who do not need a hospital admission.
- Creating elective hubs for people whose treatment involves an admission to hospital.
- Creating centres of expertise for complex elective admitted care.
- The enablers of change critical to transforming care.
- Addressing the residual backlog of patients waiting.
The drivers of rising demand for elective care, and ensuring people are receiving the right care
Given the challenge of keeping up with rising demand for care, understandably the first question asked by many healthcare leaders is whether the requirement for services should be increasing 3.8 per cent each year, or whether services can reduce this. Ageing is a big driver for growth – people aged over 65 account for three times as much elective care than people aged under 65 – and the population will continue to age sharply over the coming years.
The health of those under 65 is also a driver for growth, with increasing levels of long-term conditions in children, young people and working-age adults, for example 36 per cent of working-age adults now live with one or more long-term conditions compared to 31 per cent five years ago. Supporting people to live healthier lives through proven interventions, such as exercise-based programmes to reduce obesity, will curb the need for elective services, improve the years people live in good health and maintain their economic contribution to society for longer.
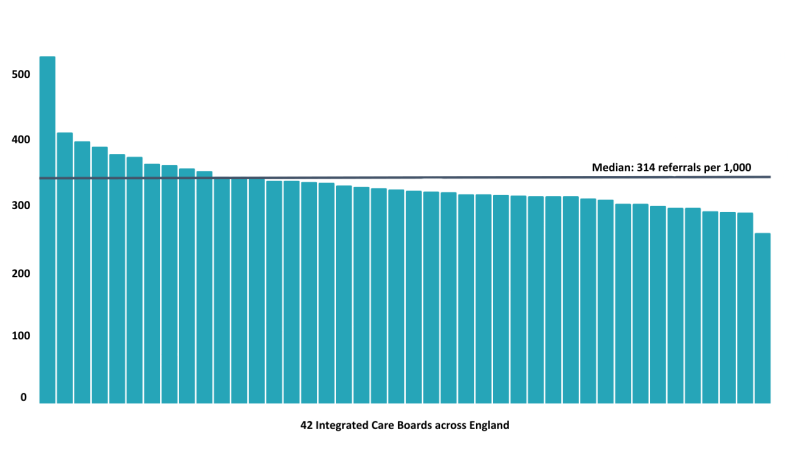
However, there is also considerable variation in the requirement for care not entirely explained by age or health status – a 5 per cent reduction in referrals could be achieved nationally if all integrated care systems (ICSs) above the median achieved median rates of referrals – see Figure 14.
Figure 14: Variations in referral rates (‘clock starts’) per 1,000 weighted population by ICS area, 2023/24
Source: NHS Referral-to-Treatment Statistics, CF analysis.
This suggests there is an opportunity to reduce the numbers of people joining the waiting list, particularly for those that go on to receive outpatient care only. The main initiative linked to achieving this is the wholesale provision of advice and guidance for general practitioners, by specialists. Timely and easy access to this advice, via telephone or digital channels, enables GPs to assess the need for a referral to a specialist consultant, or alternatively to decide on a different course of treatment.
However, people living in deprivation receive less planned care than they should and are joining the waiting list at a lower rate than the rest of the population. People living in deprivation are also 29 per cent more likely to have an emergency admission and 9 per cent and 5 per cent less likely to have day-case admission and planned overnight admission – see Figure 15. Outcomes and experience for people living in deprivation should be improved through new approaches that result in equal access to planned care. Action on this issue would therefore make referrals to the waiting list increase.
Figure 15: Activity split by Core20 population and remainder of population. Core20 is the most deprived 20 per cent of the population as identified by the national Index of Multiple Deprivation (IMD)

Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, CF analysis.
Consequently, observed healthcare speciality growth rates (which aggregate to 3.8 per cent), have been used for this report to model future capacity requirements for elective services. However, that is not to say that integrated care systems should leave demand unchecked. Where referral levels are high, proactive approaches to supporting general practitioners will ensure that patients access the most appropriate services for their needs, including through means other than referral. Conversely, where referral levels are low in areas of deprivation, proactive approaches to understand and address barriers to access and as a result encourage access to planned care. With more in-depth analysis – as part of local system planning by integrated care boards (ICBs) – more nuanced and targeted growth rates at a healthcare speciality level should be applied.
Digitalising waiting-list management and continuously validating the PTL
For the NHS to calculate whether the 18-week standard is being met in relation to each individual on the wait list, there is a need to measure when that person was first referred for secondary or consultant-led care. This point is known as the wait time ‘clock start’. The time at which the treatment has ended is known as the ‘clock stop’.
‘Clock start’ and ‘clock stop’ data is outdated and poor-quality, leading to erroneous entries requiring manual corrections. Clinical and technical validation are already occurring across many NHS providers, in part enabled by the investment made into the Federated Data Platform (FDP) and associated tools. Wholesale improvement of waiting-list management poses a significant opportunity to reduce the size of the wait list by removing people for reasons other than treatment (known as the ROTT rate). Realising this opportunity requires investment in data quality, digital infrastructure and training for staff to adopt new management practices.
If the 7.6 million people currently on the waiting list had their reason for treatment validated, around 770,000 care pathways would be removed (c.10 per cent) – due to administrative error rates and genuine reasons to remove someone without treatment. This includes patients who have changed their mind about having surgery, moved out of the country, have decided to access private care, are unfit when reviewed at pre-operative assessment, or who have died. Following a step change in approach, there is a continuous opportunity for an ongoing rationalisation of 3 per cent of the number of ‘clock starts’ every year – which is equivalent to 4.5 million over the period 2024/25 to 2028/29.
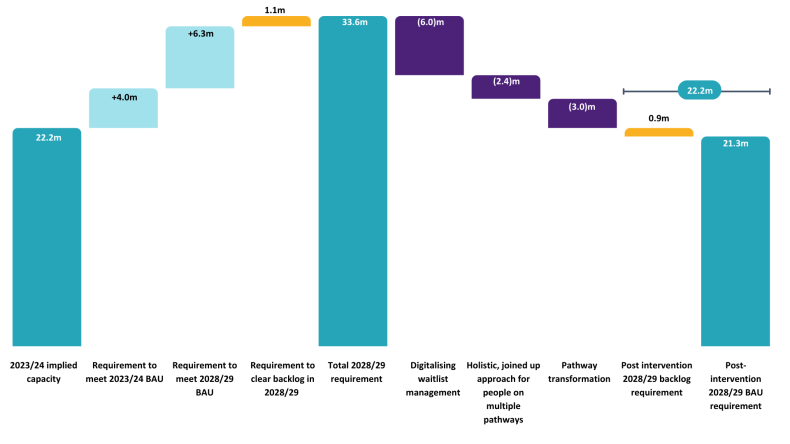
The impact of digitalising waiting-list management and continuously validating the PTL will reduce the activity requirement to address the BAU and backlog in 2028/29 by 6 million outpatient appointments, 720,000 day case procedures and 190,000 overnight stays. This represents an 18 per cent reduction in all activity types against the 2028/29 total requirement.
Transforming outpatient elective care, for people who do not need a hospital admission
Eight out of ten care pathways on the current waiting list are for people who need planned specialist care, but do not need a hospital admission, i.e. they can be seen on an outpatient basis.
Viewing people as ‘clock starts’ perpetuates a system that does not always orientate to holistic, joined-up care. It also creates a false impression of the number of individuals on the waiting list. For example, some people require more than one healthcare treatment, and their name appears multiple times in waiting lists, even though each ‘clock start’ is essentially another record related to their care as an individual. The nationally published RTT statistics show that 16 per cent of people on the waiting list appear more than once and therefore could benefit from more integrated, holistic care, involving fewer appointments and resources. This could occur through appointments involving a multi-disciplinary team approach. This approach would also improve the individual’s experience of receiving care, as it would be more personalised and less wasteful of their time.
The analysis also suggests that people on the wait list more than once typically have two open pathways and are almost exclusively receiving outpatient care only. For each non-admitted pathway, people have on average 1.4 outpatient appointments, and therefore those with two open pathways have on average 2.8 appointments. By taking a more holistic approach, the number of appointments that each person receives lessens, with an assumption that this could be reduced to 1.8 appointments (equivalent to a 35 per cent reduction in appointments), when accounting for the additional needs these individuals may have. This has the potential to reduce the number of outpatient appointments required by 2.4 million, equivalent to a reduction of 7 per cent against the 2028/29 total requirement.
Beyond a more holistic efficient model of care, increasing the number of people who receive treatment in an outpatient setting is a critical action. There is significant opportunity for the NHS to adopt the latest technology and innovation to transform outpatient care, including process automation, the application of artificial intelligence (AI) and robotics. Based on what is already in place locally in each ICS, systems could consider including:
- electronic referral management and triage
- intelligent booking, spanning from text reminders to using AI to identify likely did-not-attends
- digital advice and guidance, and virtual appointments
- process oversight to ensure necessary diagnostics are completed before appointments
- digital capacity management for outpatient clinics, and dynamic review and allocation of capacity to specialities with large outpatient waiting list requirements
- patient-initiated follow-up and remote monitoring to determine the need for additional appointments
- self-management of chronic disease through the use of digital applications.
Most of these solutions have been part of NHS England’s Outpatient Recovery and Transformation Programme, however, their consistent national implementation has not been achieved. The single biggest barrier to achieving this is access to holistic integrated patient-level data and reliable technology, which is impacted by low levels of capital spending in the NHS, particularly on IT. Investment in the required infrastructure will be essential. Having access to data, the right environment and kit and associated training to use it optimally will also have a significant impact on staff morale.
The systematic delivery of these initiatives has the potential to tackle at least the remaining 3 million additional outpatient appointments (equivalent to a reduction of 9 per cent of the total 2028/29 requirement) required to clear the backlog and meet the 2028/29 BAU requirement – see Figure 16. It actually has the potential to go further and in so doing release resources, including clinical time, for the delivery of procedures. Detailed best practice pathways, robust planning, investment in proven technology and effective change management processes that track benefits are all needed to realise the maximum potential benefit.
Figure 16: Impact of opportunities to transform waiting-list management and outpatient care over the next five years
Source: Hospital Episode Statistics – Hospital Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis
Creating elective hubs for people whose treatment involves an admission to hospital
The concept of elective hubs is long standing – the policy stems back to the 1997 Labour government’s NHS Plan, which sought to establish completely dedicated elective treatment centres providing quicker access to common procedures. This included independent sector treatment centres (ISTCs) to provide services to NHS patients, which were owned and run by non-NHS providers. The benefits of elective centres were again highlighted in High Quality Care for All in 2008. By 2010, over 90 elective centres, run by both NHS and independent organisations, were providing planned care to NHS patients. Similar numbers are operating today, but responding to the COVID-19 pandemic has reignited the mission with a further 40 hubs planned.
Elective care hubs have ringfenced capacity and staff for planned procedures, which means they are protected from last-minute postponements due to emergency care demands. These hubs are ideal for high-volume, low-complexity (HVLC) surgeries, such as cataract removal, hernia repairs and hip replacements, as well as day-case activity that does not require an overnight stay. The existing gold standard – as set by the national Getting It Right First Time (GIRFT) programme – is for these hubs to operate six days per week, 48 weeks per year, with 2.5 four-hour sessions per day, and a theatre utilisation of at least 85 per cent. While the concept has been in existence for many years, the operating model for elective hubs should be developed so the challenges of the current situation can be best met – for example elective hubs will need to use capacity flexibly for different specialities over time, including accommodating longer-term growth.
There is a proven case for delivering planned care through dedicated ‘cold’ sites:
- Safety: fewer surgical operative and post-operative complications, lower lengths of stay overall and reduced risk of hospital-acquired infection.
- Efficiency: dedicated sites allow for more intensive use, as all admissions are scheduled and will not be disrupted by emergency activity, including the extended pressures on capacity that happen every winter.
- Predictability: the scheduled nature of the site means that every bed and theatre space can be occupied appropriately, leading to better resource use.
- Enhanced patient experience and choice: through a more reliable and tempered environment.
- Better staff experience and training: clinicians get a chance to work in both unplanned and planned settings, creating training opportunities and ability to specialise, reducing pressure and burnout.
Analysis of elective hubs across the NHS suggests that only a fifth of appropriate activity is currently taking place on a ‘cold’ site – see Figure 17. Given this has been the strategic intent since the early 2000s and the benefits case has been clearly made, an accelerated programme of hub development should take place. Elective hubs should be the default option for those needing a HVLC procedure or a day-case procedure, except where the person needing care does not meet the criteria – due a risk assessment of the individual as opposed to the procedure. Consequently, a good planning assumption is a maximum of 85 per cent of all HVLC activity and 90 per cent of day case activity can take place on a ‘cold’ site. This is because some people will require additional support due to their underlying physical health, rather than because of the procedure they have, for example those with BMI >40 or poorly controlled co-morbidities such as diabetes or high blood pressure.
Figure 17: The high volume, low complexity and day-case activity – expressed as a percentage of care and volume – that took place in an elective hub between 2018/19 and 2023/24
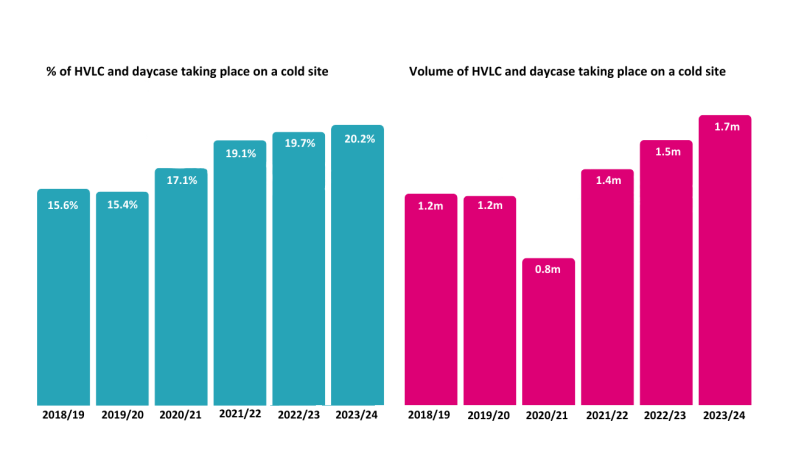
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, CF analysis.
If the NHS is to embrace the benefits of elective hubs and meet anticipated BAU demand in 2028/29, an additional 730 theatres and 3,800 beds would be needed at ‘cold’ sites. This is an 88 per cent increase in theatre capacity against the implied 2023/24 baseline of 826 theatres, and a 135 per cent increase in bed capacity against the implied 2023/24 baseline of 2,800 beds.
In setting out the requirement, it is assumed current best practice is delivered from current facilities as well as new hubs, including:
- the British Association of Day Surgery’s overnight to day-case opportunity is realised – resulting in a 3 per cent increase in day-case beds and a 14 per cent decrease in overnight beds
- the length of procedures can be shortened in elective hubs by 7 per cent for all procedures
- the GIRFT gold standard is delivered, meaning 72 per cent more procedures can be delivered through current capacity.
Making the required 2028/29 capacity available at an earlier point in time will allow some of the current backlog to be addressed. By embedding best practice and pre-empting the expected growth in this way, excess capacity in the intervening years can be used to reduce the one-off backlog of people waiting. Assuming that the capacity is in place and operational by 1 April 2026, this would support reducing the HVLC and day-case backlog by 60 per cent overall in the intervening years. With this approach, it is estimated that the non-recurrent backlog for HVLC and day-case activity will be worked off in five out of 22 specialities nationwide including dermatology, rheumatology and cardiothoracic surgery. In some regions, further specialities can work off backlogs – see Figure 18.
Figure 18: HVLC and day case one-off requirement that can be fully worked off with the proposed approach (and BAU in 2028/29 met)
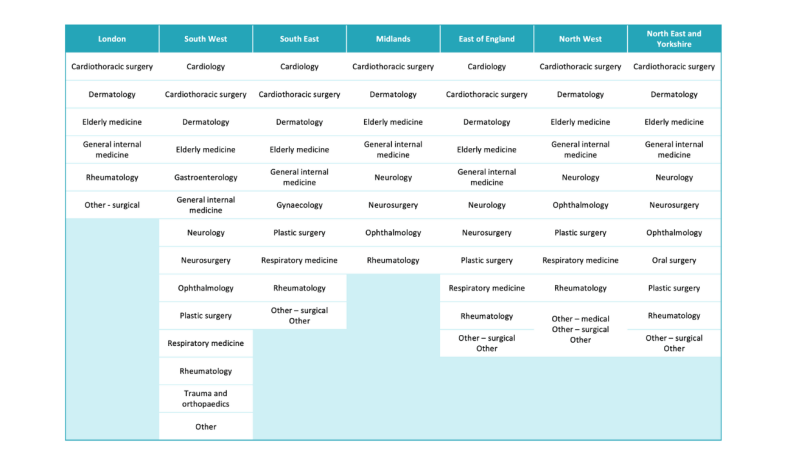
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis.
To deliver on this, a five-year strategic plan with detailed population-based demand and capacity analysis is crucial in each integrated care system. Pan-system planning should occur where needed, to take into account economies of scale (noting the size of systems is varied across the country). For instance, where there is low patient demand an elective hub could serve a larger geographical area. Collaboration between integrated care boards and providers in the NHS and the independent sector, as well between providers of all kinds, will be essential. Competitive relations are an inhibitor to the rate of progress required. Instilling collaboration is critical, not only at board-level but also between clinical teams.
Nationally, capital investment requirements need attention and approval processes need streamlining, as do the processes for making service changes (which currently take years), so that the rate of change can be radically accelerated. Support – as opposed to assurance – should be the focus, so that there is a unified and aligned approach to transforming services from national decision-makers through to clinical and operational teams.
To implement this successfully, payment and incentive models need to be carefully thought through. Incentives should be developed that encourage the outcomes sought and maximise efficiency across the whole care pathway, as well as separated elective and emergency activity. In achieving this, care needs to be taken to ensure contrary effects are minimised. For this to be possible, a detailed data-driven view of activity cost is needed at the patient-level for pathways of care, as well as an understanding of the minimum efficient scale of elective hubs. The complexity and importance of this issue means national pricing is required, starting with episodes but moving rapidly to pathways. Integration between this thinking and system planning is essential for coherence.
It goes without saying that this is a major change programme for the NHS, the like of which has never been fully and consistently achieved before. The evidence base on the management of change – including the human and organisational behavioural factors – need to be tended to and the process needs to be resourced appropriately, with the necessary capabilities and development support for the task.
Creating centres of expertise for complex elective admitted care
Delivering most HVLC procedures and day-case operations at elective hubs (‘cold sites’) also creates capacity on ‘hot’ sites, both to decompress them from high occupancy levels enabling better care for emergency patients, and to provide capacity for complex planned care.
Delivery of complex planned care often requires access to resources such as intensive care units (ICU) or co-location with other services. For example, complex breast surgery requiring reconstruction needs breast and plastics surgeons to be co-located. Therefore, this must generally be delivered from ‘hot’ sites or more than likely, large tertiary hospitals where the co-dependencies exist. Some large tertiary and quaternary centres are focused on planned care, such as Great Ormond Street, St Bartholomew’s and Guy’s Hospitals in London (to name a few) – to get to this scale, patients will come from a wide geographic area. In the main, however, hospitals are managing both emergency and planned care. Sites are often overcrowded, causing delays and reductions in patient experience – and yet the hospitals have services that do not need to be located there. The optimal configuration of services between sites also has the potential to deliver further benefits through the creation of centres of expertise. This involves consolidating complex activity with clinical co-dependencies in a way that takes advantage of the breadth of expertise across organisations (groups of hospitals) and eliminates unwarranted variation.
The creation of centres of expertise allows for the concentration of both clinical and academic capability, facilitating innovation and the adoption of emerging best practice. The benefits of this model include:
- quality and outcomes: it is well recognised that higher volumes of activity create the opportunity for greater specialisation, and through this an improvement in patient outcomes and a reduction in practice variations.
- cross-specialty care: bringing different specialisms and professions together with complementary skills delivers more effective care improving both outcomes and experience.
service resilience: strengthened rotas that are stable and fully staffed are more likely to address common workforce gaps. - participation in research: more advanced and interdisciplinary research can be conducted by concentrating infrastructure, capabilities and expert workforce in a centre of expertise. It also facilitates widening access to participation in clinical trials.
- experience for staff: centres of expertise provide more consistent and improved training and education opportunities, with clinical expertise and mentorship more concentrated among doctors, nurses and theatre staff. This results in more intensive coaching opportunities, and opportunities for specialisation.
The most common concern with centres of expertise, beyond the practicalities of change, is access for patients and their families or carers. Public engagement through polling and service change consultations consistently finds that most people are willing to travel further for the benefits outlined. 4 However, for people on lower incomes and living in poverty, transport does need consideration to ensure equity. Various approaches have been established across the NHS, but a consistent offer of patient transport for those that need it – and free travel for family members – would go a long way to mitigating travel impacts.
A further concern is the potential erosion of capabilities in district general hospitals. However, shared rotas are increasingly common, particularly in organisations that operate as part of a group, and even where group models are not in place, they have been adopted for other similar services such as in the establishment of hyper acute stroke units. 5 Far from eroding skills, when implemented well, centres of expertise have the potential to enhance capabilities by providing diversity of experience. Furthermore, having stable fully staffed rotas creates an environment in which further service developments can flourish, including increased teaching, learning and career development opportunities.
Taking this approach, by 2028/29, the BAU requirement for complex elective care could be completely delivered, within existing capacity assuming 85 per cent of HVLC activity and 90 per cent day-case procedures were delivered at elective hubs. By embedding best practice and pre-empting the expected growth, excess capacity in the intervening years can be used to reduce the one-off backlog of people waiting. Assuming that the capacity is in place and operational by 1 April 2026, the complex overnight non-recurrent backlog will be worked off in all specialities in all regions.
Without transformation in the way elective care is delivered, rising demand driven by the changing demographic profile of the population means there is insufficient capacity within current facilities to deliver the complex activity required. Expansion of protected elective capacity for complex care in major hospitals is needed to address the shortfalls, or waiting times will rise. Major hospitals do not necessarily need to expand overall, if elective hubs are created, but they do need to be remodelled and refurbished to enable efficient care delivery. In urban areas, adoption of large-scale elective centres for complex care – like those that exist in London (and elsewhere) – could also be considered, concentrating complex planned care requirements onto sites as opposed to mixing elective and emergency flows.
Improvements in the delivery of admitted elective care through the establishment of both hubs and centres of expertise need effective working with local authorities to ensure seamless access to social care for those that need it to be discharged home safely. However, overall reductions in waiting times, increasing day-case procedures and safer, higher-quality environments will lessen the care requirement as people will be fitter both before treatment and on discharge.
Creating centres of expertise requires a five-year strategic plan, similar to the planning required for elective hubs, with interconnected analysis. Integrated care boards and NHS England, as the commissioner of specialised services, need a combined approach to population-based demand and capacity planning, resulting in a shared plan for each system. The smaller scale of these services will also necessitate greater pan-system planning.
Taken together the establishment of elective hubs and centres of expertise for complex elective care will transform the efficiency of care delivery. They make planned care requiring a hospital stay more streamlined, of higher quality, and in dedicated facilities. The result is a reduced requirement for bed and theatre capacity, with staff delivering more operations in the time they have available.
With no interventions, the requirement for elective beds, both overnight and day-case, would increase to 15,000 in 2028/29 from current implied capacity of 10,500 in 2023/24 (a 43 per cent increase). Implementing waiting list validation, elective hubs and centres of expertise for complex elective care would reduce this requirement by 3,900 beds, and a further 0.4k beds would be needed temporarily until 2028/29 to address the one-off backlog requirement. As a result, by 2028/29, 200 additional beds would be needed. However, the configuration of these beds between hot and cold sites would need to materially change. 3,800 more beds would be needed at cold sites (a 135 per cent increase), and 3,600 fewer beds would be needed for elective care at hot sites (a 47 per cent decrease), meaning that occupancy levels could be reduced to improve emergency flow – see Figure 19.
Figure 19: Elective bed requirement in 2028/29 – before and after implementation of opportunities – against current capacity
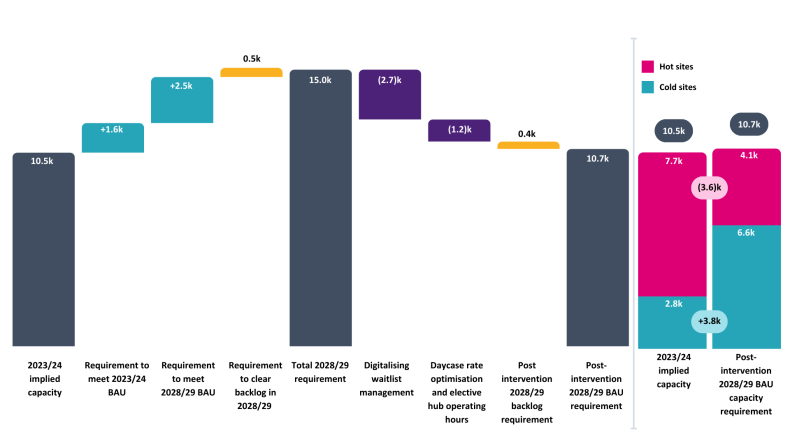
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, NHS Referral-to-Treatment Statistics, CF analysis.
With no interventions, the requirement for elective theatres would increase to 4,500 in 2028/29 from current implied capacity of 3,200 in 2023/24 (a 41 per cent increase). Implementing waiting list validation, elective hubs and centres of expertise for complex elective care would reduce this requirement by 1,200 theatres, and a further 120 theatres would be needed temporarily until 2028/29 to address the one-off backlog requirement. As a result, by 2028/29, 52 fewer theatres would be needed overall. As with the bed requirement, the configuration of these theatres between hot and cold sites would also need to materially change. 720 more theatres would be needed at cold sites (an 88 per cent increase), and 770 fewer theatres would be needed for elective care at hot sites (a 33 per cent decrease) – see Figure 20.
Figure 20: Elective theatre requirement in 2028/29 – before and after implementation of opportunities – against current capacity
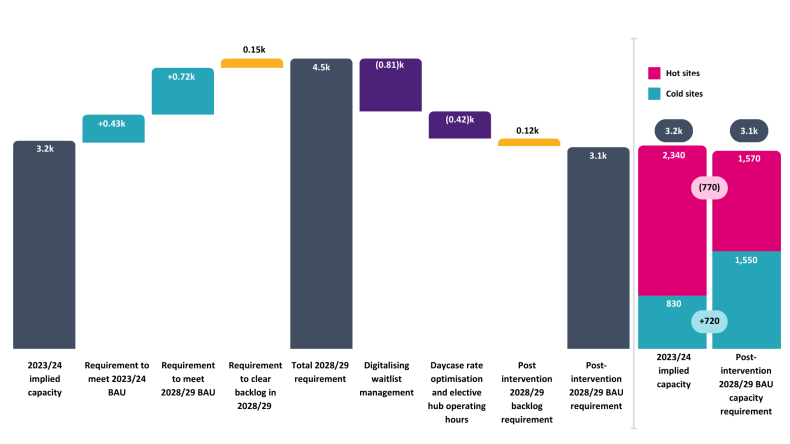
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity, NHS Referral-to-Treatment Statistics, CF analysis.
Delivering transformation to pathways of care with a focus on the enablers of change
While many of the enablers for change and transformation have been touched on throughout the report, they are foundational to success and the scale of effort required should not be underestimated. In this section, the requirements are drawn together to set out the different aspects that need to be considered.
Long-term, aligned planning that is reviewed regularly
Strategic planning is needed at different levels of the NHS architecture and these plans should align so they are mutually reinforcing. Demand for services is evolving. NHS England and ICBs will need to monitor this to predict changing requirements, and to ultimately ensure the right capacity is consistently in place where it is needed, including shifting resources towards earlier intervention and prevention. NHS, central and local government processes for oversight and decision-making should be united with the strategic intent and should facilitate rapid progress. Excessive layers of bureaucracy that impede services from adopting best practices or responding to changing population needs should be stripped back.
Capital investment that facilitates change
Capital is required to establish elective hubs and to enable some reconfiguration of services for centres of expertise for complex elective care. It is also needed universally to enable the widespread adoption of advanced technology. Access to capital has acted as a barrier to change for some time, and consequently capital is also needed to clear the maintenance backlog. A refreshed approach – affording greater flexibility (and certainty) at the local level, coupled with fast-track decision-making processes – would have a positive impact. NHS leaders estimate that, to boost productivity growth by 2 per cent per annum, an additional £6.4 billion a year is needed over the next Spending Review cycle to clear the maintenance backlog and invest in modern technology and estate, including community diagnostic centres and elective hubs. The NHS itself also does not need to provide all the capital if it partners with the private sector in the delivery of services, providing long-term commitments are sufficient for other operators to secure debt and warrant investment.
Funding, payment and incentives that relate to the outcomes desired
Nationally, incentives need to be created to optimise outcomes and efficiency across the whole pathway of care. They should encourage best practice and enable the best locations for care delivery, including separated emergency and elective care. They must also avoid unintended consequences, like rewarding poor-quality estates. The approach should encourage both NHS and independent providers to deliver elective hubs and encourage collaboration between organisations. Outcomes-based payments help to incentivise allocative and technical efficiency. This requires a review of prices assigned to activity and then the development of whole pathway models. A detailed data-driven view of activity cost is needed at the patient-level for pathways of care, as well as an understanding of the minimum efficient scale of delivery.
Workforce planning aligned to demand and linked to transformation opportunities
A critical enabler will be workforce and having the right number of staff aligned to elective care. A significant limitation is the current data environment and the quality of data within the NHS. For example, there is no activity-based workforce data available, which means that the relationship between staff and the delivery of care is unknown. It is therefore impossible to know for certain what impact the opportunities will have on the workforce requirement, or what the workforce requirement to deliver on the opportunities set out in this report are. However, as best practice pathways are defined and incentivised, processes are digitalised, environments are modernised to allow efficient practices and collaborative and shared workforce models are embraced, the workforce requirements should be clarified. This will need active working through in order fully to understand them by geography and speciality.
Fostering clinical leadership and accountability
Clinicians that take accountability for creating, deploying and achieving efficient pathways of care – in partnership with operational managers – is the most powerful model for delivery. Clinical engagement with administrative processes will strengthen relationships and encourage real-time discussions that support effective operational planning. Re-engaging clinical leadership, providing structured training and development opportunities, and recognising and rewarding the contribution made is vital.
High-quality booking and scheduling for patients and staff
Booking and scheduling should be user-friendly and inclusive, with a service orientation. Whether in conversation or online, information needs to be accessible and easy to navigate for patients and staff alike. Its criticality to the efficiency of care pathways needs to be promoted, recognising excellence is intimately linked to a patient’s experience of care and to a hospital’s productivity level. Championing the administrative and clinical staff that underpin the process, providing training and development, and encouraging widespread digital adoption will make it easier for everyone.
Continuous improvement to data quality and the widespread adoption of digital innovations
Widespread use of data is essential to inform decision-making, from policy, planning and pricing to the delivery of care. Better data will also improve the effectiveness of technology and AI. There should be wholesale adoption of proven applications and tools that improve interactions with patients, as well as those that improve care and management processes. All parties need to fully embrace data and digital to understand pathways of care, manage workflows effectively and optimise the use of scarce resources. This requires integration of electronic health record with workflow tools – across the NHS and independent sector from referral through to follow-up. In so doing, the recommendations of the Hewitt review should be embraced.
Staff and team training and development to enhance improvement capabilities
Years of declining performance and overwhelming pressures have led to a loss of the skills needed to consistently meet standards and stay patient centred. Capabilities need to be rebuilt to deliver improvements at scale. This includes collaborative commissioning of the right services for the needs of differing populations and settings, the transformation skills to prioritise and develop impactful solutions, and the change management skills, behaviours and mindsets that are needed to see these translated into sustained practice. Finally, once new care models are in place, pathway management skills across the whole multidisciplinary team are needed to ensure the consistent daily delivery of care.
Addressing the residual backlog of patients waiting
If all the above steps are achieved, for some healthcare specialties, the non-recurrent backlog will be addressed and the 18-week standard met within five years, through early adoption of the capacity requirement. However, this approach alone will not be enough for other specialties – see Figure 21.
Figure 21: Residual backlogs by healthcare speciality and region where the backlog will not be worked off within five years
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis.
Additional funding, staff and resources will be required to address the outstanding backlog in these healthcare specialties. There are three main ways of addressing this issue:
incentivise NHS staff to undertake additional work over and above their normal schedules
use insourcing providers to make additional use of NHS capacity out of hours
outsource activity to private healthcare providers using speciality-level volume-based contracts.
A combination of the three approaches is likely required. As this is a non-recurrent backlog and not the ongoing BAU requirement, expanding NHS facilities to address this need would create excess capacity over the longer-term and hence would not deliver best value.
Chapter footnotes
- 4. Picker Institute, ‘Patients’ experience of CHD Choice’, 2003; Cancerbackup research, ‘Cancer Research Part Two’, May 2007. ↑
- 5. A group is an organisational form which brings together multiple provider organisations with an organisational model which has a ‘central headquarters’; discrete and locally managed ‘operating units’; standardised systems, practices, and protocols set by the central HQ and implemented at each operating unit; and a culture and value-set that is shared across the Group. ↑
Conclusion
The challenges in meeting the 18-week constitutional standard are long-standing. They were significantly exacerbated by the pandemic, but not caused by it. Today the waiting list stands at 7.3 million and it will grow to 8.3 million by 2028/29 if current growth in referrals continues at 3.8 per cent in aggregate. Assuming no further progress in the transformation of care delivery, the NHS will need to provide 33.6 million outpatient appointments, 4 million day-case procedures and 1.1 million overnight stays to clear the wait list back to levels that would sustain 18-week performance in 2028/29. This is 50 per cent more activity than is currently being delivered. If the aim is to offer the public a reliable commitment to starting care within 18 weeks of a referral, bold and decisive change is needed to transform elective care.
Taking all of the opportunities in this report together, the overall impact on the activity requirement means that from a position of needing 11.4 million more outpatient appointments, 1.2 million day-case procedures and 340,000 overnight stays annually, the NHS would move to needing no additional further outpatient appointments, 600,000 more day-case procedures and 50,000 more overnight stays in 2028/29 – see Figure 22. Hence, if all the opportunities identified were delivered, the government’s early promise of an additional 2 million appointments, operations and diagnostics a year would deliver the additional requirement (noting that diagnostics is not included within this analysis).
However, the additional activity needs to be focused on operations and coupled with major change. While improvements are underway across the country, major transformation is required in the way care is planned and delivered. Most radically elective hubs need a significant programme of expansion alongside the wholesale creation of centres of expertise for elective care. To achieve this alongside the other necessary changes outlined in this report requires significant investment, energy and government commitment to make it happen.
Figure 22: Elective activity requirement in 2028/29 – after implementation of opportunities compared to current activity levels
Source: Hospital Episode Statistics – Hospital Admitted Patient Care Activity and Outpatient Activity, NHS Referral-to-Treatment Statistics, CF analysis.